Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
|
|
Aleksandra ZarzyckaRoyal HaskoningDHVEindhoven University of TechnologyThe Netherlandsal.zarzycka@gmail.com | Wim MaassenRoyal HaskoningDHVEindhoven University of TechnologyThe Netherlandswim.maassen@rhdhv.com | Wim ZeilerEindhoven University of TechnologyThe NetherlandsW.Zeiler@tue.nl |
The health care sector is highly energy
intensive. Worldwide, circa 6% of the total energy consumption in the buildings
sector is represented by energy usage in medical centres. For this reason,
hospitals strive to reduce their consumptions and CO2-emissions. In
order to meet the requirements, set by the European Union Energy Performance of
Buildings Directive (EPBD), all buildings (residential and utility) need to
comply to Nearly Zero Energy Building requirements according the EPBD [1].
Previous study [2] has looked into energy consumptions of various spaces within
a hospital and concluded that for Dutch hospitals the energy reduction
potential seems to be the highest in isolation rooms and operating theatres
(OTs). For the OTs the highest energy consumption is attributed to the amount
of supplied air, energy used for fans and the time that surgery rooms are in
operation.
In this study the possibility to reduce energy
consumption in the OTs is investigated, using an approach that puts the human
and his safety in the centre of attention. Most important factors in infection
prevention are therefore categorized into four groups, the so called ‘four Ps’:
pathogens, people, practice and place (Figure 1). In the
Netherlands, a commonly used approach for an energy-efficient building design is
the three-step strategy called ‘Trias Energetica’ [3]. Due to increasing
concern and evolution of techniques, the ‘Trias Energetica’ has been upgraded
to a ‘Five-Step Method’ [RHDHV], as can be seen in Figure 2.
The additional steps to the original approach are: user demand and behaviour
(point 1) and energy exchange and storage systems (point 4). The former step
implements the ‘user-oriented’ concept through smart building designs and
controls. The focus on the user and his primary process results in possibilities
for improvements of indoor climate as well as productivity. Furthermore, it can
substantially decrease energy use. This idea is further developed in this
research. By investigating the parameters needed to create a safe environment,
starting from the most basic layer such as bacteria transmission, the project
aims to draw conclusions on the actual requirements for a healthy indoor
environment in the OT, questioning the current standards. Is such a high air
exchange rate necessary? Are current systems the most efficient infection
prevention methods? How can the OT be optimized for a high surgical
performance? These questions can only be answered by understanding the actual
needs of this specific environment, therefore the focus on user demand and behaviour
is crucial.
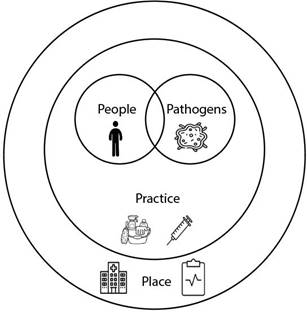
Figure 1. Four “Ps” of infection prevention.
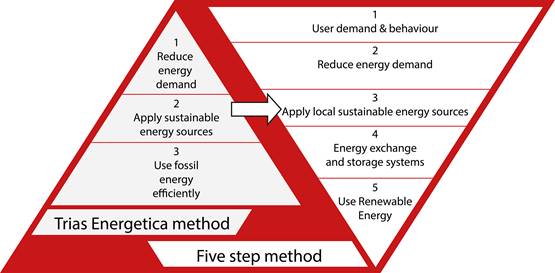
Figure 2. Building design approaches: ‘Trias
Energetica’ versus the upgraded ‘Five Step Method’.
The total
annual number of patients that suffer from surgical site infections (SSIs)
amounts to 1.12% for European hospitals [4]. Inside the operating theatre, bacteria can reach the wound either by
dislocation within patient’s own microbiota, through air or from poorly
disinfected tools. The shedding of bacteria from staff’s skin is
considered one of the biggest potential sources of wound contamination [5].
Each person sheds around 10,000 skin particles per minute into the air while
walking. Approximately 10% of these are estimated to carry bacteria [6]. Skin
fragments carrying bacteria have an average size of 12 μm (range
between 4-60 μm). Surgical-site contamination by airborne particles
is ascribable in 30% of cases to direct settling of the particles on the wound
and in 70% of cases to settling on the instruments and surgeon’s hands followed
by transfer to the wound [7].
There are
several environmental factors that may impact the infection acquisition, from
which four are of relevance in the operating theatre: relative humidity (RH),
temperature, air speeds and movement intensity of the particles. There is
research showing that maintaining the humidity levels in the range between 40
and 60% can be related to decreased infection rates in hospitals [8],[9]. This
is due to lower possibility of droplets to remain suspended in the air for
prolonged periods of time, prevention of mucous membrane from drying out,
shorter life span of bacteria and viruses in such conditions and lack of
accumulation of static electricity with higher humidities [10],[11].
On the
other hand, professionals argue that relative humidity is not of such
importance and there is no need to pay close attention to its levels.
While the
primary focus of indoor environment in operating theatres is on infection
prevention, thermal comfort of the workers tends to be generally overlooked.
Study performed by Ilse Jacobs focused on the thermal sensation of surgical
staff members in OTs equipped with different ventilation systems [12]. The
conclusion of the research was that surgeons tend to feel from slightly warm to
hot, anaesthetists and nurses from slightly cool to cold, and the patient from
slightly cool to very cold. Only the surgery-assistant experiences a
comfortable environment with the current environmental and clothing parameters
according to Van Gaever et al. [13].
When it
comes to the patient, a study by Khodakarami et al. stated that the temperature
must not drop below 21°C [11]. However, a temperature above 23°C already
becomes intolerable for the surgical staff. During an operation, body
temperature is lowered due to open body wounds, infusion of cold fluids,
inhalation of cold gases and lowering muscle activity or because of the
pharmaceutical agents given to the patient. Even mild hypothermia can lead to
numerous complications, which might lower the resistance to surgical wound
infection [14]. A 36% decrease in infection rates was observed by Melling in
patients who received some form of warming during the surgery [15].
In an
environment where anaesthetic measures are suppressing immune system of a
patient and a direct contact between him and OT staff is frequent, failure to
maintain highest standards of (hand) hygiene can result in increased infection
risk.
Table 1 summarizes factors associated with
surgical-site infections. The icon representing a group of people means that a
factor is related to discipline. Icon with a piece of paper shows the
connection to rules and regulations. Icon with a light bulb means the relation
with the skills of the operating team.
Table 1. Factors associated with surgical-site
infection.
Operation
characteristic | |
| Inadequate surgical team
preoperative hand and forearm antisepsis |
| Inappropriate or untimely antimicrobial prophylaxis |
| Inadequate sterilization of
instruments |
| Contaminated OT environment |
| Inappropriate surgical
attire and drapes |
| Inadequate preoperative skin preparation |
| Inappropriate preoperative
shaving |
| Poor surgical technique: excessive blood loss, hypothermia, tissue
trauma, entry into a hollow viscus, devitalized tissues etc. |
| Excessive duration of
operation |
Table 2 shows an overview of some of the
factors that influence the occurrence of surgical site infections. It has to be
noted that these values vary between studies and very often it is hard to
estimate their role in reduction of SSI rates due to complexity of the surgical
environment and too many factors that are mutually dependent. For some
positions, for example surgical clothing, such an estimation was not possible,
therefore these were not included in the table.
Table 2. Influence of various factors on the decrease
in surgical site infection rates [16],[15],[17],[18].
Influencing factor | Decrease in SSI rates |
Hand
hygiene | 13-54% |
Proper
antibiotic use | 26-92% |
Occurrence
of hypothermia | 36% |
Preoperative
showering with chlorhexidine | 24.4% |
Type of intervention | up to 83.7% |
Health
state of the patient | up to 86.4% |
Operating
theatres can be classified depending on their performance as suitable for
high-risk operations or not. Ventilation system which is installed in a given
OT is responsible for providing clean air and maintaining the quality of the
environment according to the class of the room.
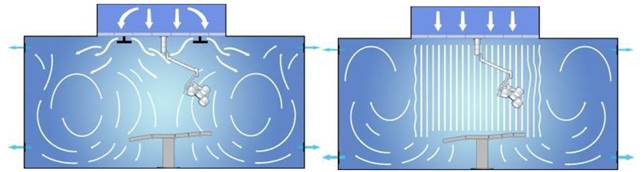
Figure 3. Flow patterns for the TMA (left)
and UDF (right) ventilation systems [12].
In general,
there are two main ventilation principles that are applied in OTs: mixing
ventilation (turbulent mixed airflow TMA) and displacement ventilation
(unidirectional flow UDF), as presented on Figure 3.
Turbulent mixed airflow supplies turbulent streams of HEPA filtered air through
diffusers on the ceiling, therefore creating a mixed ventilation in the whole
space of an operating theatre. The system is based on dilution principle, which
results in exponential decay of high concentrations of airborne microbes over
time [19]. Second type is a system supplying conditioned air in a parallel
stream to the surgical field. The streams of air move in parallel layers and,
with equal speed of around 0.4 m/s, reach the operating table. This
creates a sort-of protective curtain of airflow surrounding the surgical site.
Apart from traditional systems, recent years have seen the emergence of new
systems, based on mentioned principles. Halton Vita OT Space is a system that
has been developed on mixing principle in the year 2015 and is presented on
Figure 4 below.
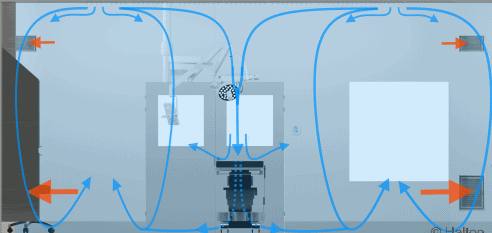
Figure 4. Halton - mixing ventilation
principle [20].
The
controlled dilution effect is created by circumferential air supply directed
both inward towards the operating area and outward towards the room periphery.
The emissions generated in the room periphery are diluted by additional air
supplied to periphery zone. Based on room dimensions, operational needs and
thermal comfort, airflow pattern can be adjusted. An example of a recently
developed system working on the principle of UDF is Optimus Integrated Surgical
Environment shown on Figure 5. In this approach the
entire operating complex is integrated into one solution, including lighting,
web cams, sensors, microphones and surgical cameras. The room air volume will
be replaced 30 times per hour at very low velocities [21].

Figure 5. Optimus Integrated Surgical
Environment – UDF ventilation principle [21].
A system
called Opragon (Figure 6) is based on a modification of
UDF - Temperature controlled Laminar Airflow (TAF). In this solution slightly
chilled, HEPA-filtered air is introduced to the room and distributed by low
impulse, half-spherically shaped air showers. They are mounted in a circle,
creating an ultra-clean zone. Outside of the zone, eight additional diffusers
are mounted on the ceiling, preventing stagnation zones in the periphery of the
room. Higher density of chilled air causes it to fall to the floor at a speed
controlled by the difference in temperature between the added air and the air
at the level of the operating table. The temperature difference of −1.5
to −3°C between the added ultra-clean air and the surrounding air in the
room at the operating table level needs to be maintained in order to guarantee
a speed of around 0.25 m/s at the operating table level [22].
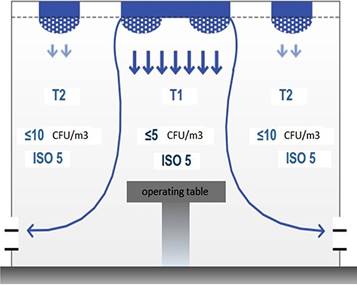
Figure 6. Opragon ventilation system based on
TAF principle.
The
temperature gradient drives the central vertical flow of cooled air. The air
showers located in the outside zone provide control of the room temperature,
therefore there is no need for additional heating system, like in a laminar
downflow. A comparison between three mentioned systems is presented in Table 3.
Having conducted the literature research by starting from the human perspective
it is possible to distinguish new strategies for energy reduction and process
improvement. Traditionally the design of the operating theatres is based on
many steady-state parameters, while in practice these values vary greatly.
Aspects such as hand hygiene, skin shedding of the staff, parameters of the
clothing (in case multi-use attire is used), movement of the staff etc. cannot
be approximated with one number since they differ everyday depending on the
team. Moreover, environmental factors such as relative humidity and indoor
temperature can play a role in the spread of pathogens. When it comes to the
systems themselves, their design parameters such as the location of inlets/outlets
or location of heat sources in the room can greatly alter the way bacteria is
transported within the OT.
Table 3. Comparison of three ventilation systems [19].
Description | Turbulent mixing | Unidirectional flow | Temperature controlled
airflow |
ISO class in the centre
of the OR (steady-state) | 7 | 5 | 5 |
ISO class in the periphery of the OR
(steady-state) | 7 | 7 | 5 |
Protected area | No | Yes | Yes |
Recovery time <3 min | No | Yes | Yes |
Type of flow | Turbulent | UDF | UDF |
Acceptance for class Ia surgeries | No | Yes | Yes |
Average airflow (m³/h) | 3 200 m³/h | 12 000 m³/h | 5 600 m³/h |
Recirculation of air | 0% | 70% | 45% |
Noise level in
empty room | 45 dBA | 58 dBA | 48 dBA |
Ventilation power | 2.8 kW | 8.0 kW | 5.7 kW |
CFU/m³median(range) | 10 (0-162) | 0 (0-16) | 1 (0-29) |
It is
therefore crucial for the engineers and designers of the OTs to be able to
understand the way that bacteria travels in space and reaches the wound area of
the patient. With better understanding of these mechanisms, ventilation systems
could be adjusted to provide more precise and more energy-efficient solutions.
However, before the research on the bacteria transmission is completed, there
are several energy saving measures that can already be implemented in the
hospitals:
·
Airflow
control based on particle concentrations,
·
Variable
temperature with the outdoor weather,
·
Turning
down the system for the night,
·
Better
planning of the use of OTs based on operation type,
·
Removing
humidification,
·
Increased
air recirculation.
One of the
energies saving measures is airflow control based on particle concentrations.
This energy saving measure at the same time provides increased infection
prevention. By putting a real-time particle counter in the vicinity of the
wound, it is possible to get an immediate feedback on the number of particles
in that area. Although there is no direct correlation between the number of
particles and the amount of colony forming units, bacteria always need a
particle on which it can settle. Therefore, we can assume that if there is no
or very little particles in the air, the chance of finding bacteria is also
very low. Having a real-time feedback enables the system to reduce the amount
of air if there are no particles in the air and increase it in case there is a
significant of particles, thus improving infection prevention. This approach is
in line with the statement that OTs design cannot be based on steady-state
parameters. By the real-time measurement, the ventilation system can be
adjusted to the current situation and its needs. Another measure is related to
changing the absolute temperature inside the OT based on the outdoor
conditions. Even though the temperature difference between the inlet and outlet
air inside the room needs to be kept the same, the absolute values can vary
with seasons, allowing for energy savings. Third measure is related to turning
down the ventilation system for the night and it has been studied by
Dettenkofer et al. [23]. The authors have concluded that shutting down OT
ventilation during off-duty periods does not appear to result in an
unacceptably high particle count or microbial contamination and if the system
is restarted 30min before the scheduled operation, high levels of air quality
will be maintained. Fourth possibility is related to improved planning within
the hospital management. Not all operations need to be conducted in the highest
performance OTs, for which the energy consumption is very high in order to
provide the highest levels of air cleanliness. If a classification of operation
types is created, they could be distributed between two performance classes of
the OTs, leading to energy savings. Last two measures are already being widely
implemented in the USA with positive results regarding energy savings.
The article
shows added value the approach was the focus on energy conservation begins
primarily with the human needs and process conditions needed to supply a
productive, healthy and comfortable indoor environment. Starting from the
essential human and process needs it leads to an analysis resulting in relevant
energy conservation possibilities.
[1] EU, “Directive 2010/31/EU of the European
Parliament and of the Council of 19 May 2010 on the energy performance of
buildings (recast),” and Directive (Eu) 2018/844 Of the European Parliament and
of the Council of 30 May 2018 amending Directive 2010/31/EU on the energy
performance of buildings and Directive 2012/27/EU on energy efficiency.
[2] I. Schoenmakers, “Increasing HVAC energy
performance in University Medical Centres by optimizing energy efficiency
indicators,” p. 78, 2014.
[3] A. G. Entrop and H. J. H. Brouwers,
“Assessing the sustainability of buildings using a framework of triad
approaches,” J. Build. Apprais., 2010.
[4] “European Centre for Disease Prevention and
Control.,” Point Preval. Surv. Healthc. Assoc. Infect.
Antimicrob. use Eur. acute care Hosp., vol. 2013 SRC, 2013.
[5] M. A. Ritter, “Operating room environment,”
in Clinical Orthopaedics and Related Research,
1999.
[6] W. C. Noble, “Dispersal of skin
microorganisms,” British Journal of Dermatology.
1975.
[7] D. Chauveaux, “Preventing surgical-site
infections: Measures other than antibiotics,” Orthopaedics
and Traumatology: Surgery and Research. 2015.
[8] H. O. W. Radiology, H. T. O. Find, and F. L.
Diseases, “Breathe Easy,” 2016.
[9] G. J. Harper, “Airborne micro-organisms:
survival tests with four viruses,” Epidemiol. Infect.,
vol. 59, no. 4, pp. 479–486, 1961.
[10] A. V. Arundel, E. M. Sterling, J. H. Biggin,
and T. D. Sterling, “Indirect health effects of relative humidity in indoor
environments,” Env. Heal. Perspect, 1986.
[11] J. Khodakarami and N. Nasrollahi, “Thermal
comfort in hospitals - A literature review,” Renewable
and Sustainable Energy Reviews. 2012.
[12] I. Jacobs, “Thermal comfort of surgical staff
in operating rooms with different types of ventilation systems,” no. July,
2018.
[13] R. Van Gaever, V. A. Jacobs, M. Diltoer, L.
Peeters, and S. Vanlanduit, “Thermal comfort of the surgical staff in the
operating room,” Build. Environ., vol. 81, pp.
37–41, 2014.
[14] D. I. Sessler, “Mild perioperative
hypothermia.,” N Engl J Med, vol. 336, no. 24,
pp. 1730–1737, 1997.
[15] A. C. Melling, B. Ali, E. M. Scott, and D. J.
Leaper, “Effects of preoperative warming on the incidence of wound infection
after clean surgery: A randomised controlled trial,” Lancet,
2001.
[16] J. L. Alfonso-Sanchez, I. M. Martinez, J. M.
Martín-Moreno, R. S. González, and F. Botía, “Analyzing the risk factors
influencing surgical site infections: the site of environmental factors.,” Can. J. Surg., 2017.
[17] P. J. E. Cruse and R. Foord, “A Five-Year
Prospective Study of 23,649 Surgical Wounds,” Arch.
Surg., 1973.
[18] B. Friberg, S. Friberg, and L. G. Burman,
“Inconsistent correlation between aerobic bacterial surface and air counts in
operating rooms with ultra clean laminar air flows: Proposal of a new
bacteriological standard for surface contamination,” J.
Hosp. Infect., vol. 42, no. 4, pp. 287–293, 1999.
[19] M. Alsved et al.,
“Temperature-controlled airflow ventilation in operating rooms compared with
laminar airflow and turbulent mixed airflow,” J. Hosp.
Infect., vol. 98, 2017.
[20] “Halton.” [Online]. Available: https://www.halton.com/nl_NL/health/home.
[21] “Optimus Integrated Surgical Environment.
Integrated Air Plenum.” [Online]. Available: www.optimusise.com/components/integrated-air-plenum/.
[22] Airsonnet, “Opragon brochure,” 2009.
[23] M. Dettenkofer et al.,
“Shutting down operating theater ventilation when the theater is not in use:
infection control and environmental aspects,” Infect
Control Hosp Epidemiol, 2003.
Follow us on social media accounts to stay up to date with REHVA actualities
0