Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
|
|
|
|
Ilse Jacobs | Marcel Loomans | Lada Hensen-Centnerová | Michel Krombeen | HeliantheKort |
Eindhoven University of Technology, Department
of the Built Environment, Building Performance group, Eindhoven.ilse-jacobs@hotmail.com | Eindhoven University of Technology, Department
of the Built Environment, Building Performance group, Eindhoven.m.g.l.c.loomans@tue.nl | Eindhoven University of Technology, Department
of the Built Environment, Building Sustainability group, Eindhoven.l.hensen@tue.nl | Unica, Bodegravenm.krombeen@unica.nl | Eindhoven University of Technology, Department
of the Built Environment, Building Performance group, Eindhoven.h.s.m.kort@tue.nl |
In an
operating theatre, the most important requirement is that the patient receives
the best possible care during surgery. The assumption is that by efficiently
supplying sufficient clean air into the room the occurrence of post-operative
wound infections will be minimized. Therefore, the design of an operating
theatre is mainly based on air quality for contamination control (see Figure 1).
In case of an operating theatre, the possible sources of pollution are the
surgical staff, the surgical instruments and the patient itself. Because, based
on these sources, the amount of air that needs to be supplied is considerable
(in an operating theatre the air change rate is in the order of 15-30 h-1
[1]), theoretically efficient unidirectional downflow (UDF) ventilation systems
are often chosen over mixing systems.
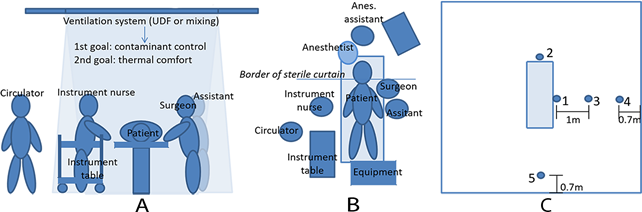
Figure 1.
View and plan of a typical operating theatre with a downflow-based ventilation
system [1A, 1B]. Figure 1C gives an impression of the typical positions of
the surgical team members (1=surgeon/assistant, 2=anesthetist,
3=instrument nurse, 4/5=circulator), where positions 1-3 are often positioned
in the direct influence of the downflow system.
Until 2014,
The Netherlands prescribed a UDF system for class I operating theatres, i.e.
highest air quality requirements. After 2014, a more performance-driven approach
was chosen which made it possible to look beyond conventional systems, offering
possibilities for new design solutions. In the entire discussion about the
quality of an operating theatre, the effect of the work environment of the
surgical staff on the result of an operation is generally overlooked. Good
lighting is self-evident and translated, e.g., into operating lamps.
Sound/speech intelligibility is a point of attention, but also thermal comfort
plays an important role in achieving an optimal work environment. This study
focused on the latter aspect. Some earlier research is available [2] and
literature also shows some numerical analysis of the thermal conditions in an
operating theatre [3]. The objective of this research was to analyze the performance of existing operating theatre
ventilation systems and new developments in this field with respect to thermal
comfort, and identify which system(s) may be preferred from a thermal comfort
point-of-view.
Figure 2. UDF (2T) [left] – Opragon [middle] – Halton [right].
As part of
the research is perception based, and limitations in the numerical analysis are
significant the work is performed experimentally. In the study, in-situ
measurements have been performed in several operating theatres with different
types of ventilation systems (see Figure 2 for an
impression). The systems studied are UDF (two-temperature [2T]
system), Opragon and Halton. The measurements have
been carried out in operating theatres in two different hospitals (UDF 2T, Opragon) and in two mock-ups
of an operating theatre at the relevant manufacturers of the systems (Avidicare [Opragon] in Sweden;
Halton in Finland). Thermal comfort measurements were derived according to ISO
7730 [4] (Predicted Mean Vote [PMV]/ Predicted Percentage of Dissatisfied [PPD]).
Additionally, non-uniform thermal comfort conditions (draught, vertical
temperature gradients, floor temperature and radiant asymmetry) have been
determined. Where possible, the measurements have been carried out for three
different use situations:
1. No subjects in the room,
2. Under static conditions (i.e. real persons
in fixed positions, or represented as heat sources),
3. Under dynamic conditions (i.e. real persons
moving around as if a real surgery is performed).
Reproducibility
of the measurements has been tested by performing similar measurements for
equal boundary conditions. The results show that DPMV ≤ 0.1 and the draught rate and
vertical temperature gradient were within the accuracy level of the applied
sensor.
In addition
to the objective measurements, subjective analysis has been performed through
online surveys on thermal comfort perception of surgical staff members during
surgeries. General thermal comfort was examined, but also non-uniform thermal
conditions such as draught. For these surveys use has been made of literature
[2][5]. This subjective analysis was performed parallel to the experimental
research.
For the
subjective part of the research, 42 Dutch hospitals (out of 81) were approached
to participate in the study. In total, 12 hospitals eventually cooperated and
survey results of 341 participants (surgical staff members) were collected. All
members of an operating team were represented in the response, while UDF
(one-temperature [1T]/2T plenums in particular) was present as a system. For
the statistical analysis of the data SPSS Statistics 25 has been used.
Significance is assumed at p < 0.05. Further
details of the research can be found in [6].
Subjective data - An example of the subjective results of the
survey is shown in Figure 3. There is a difference in
perception of the thermal conditions between the members of the surgical team.
One can derive that, on average, the staff members are feeling cold, with the anesthesiology assistant being significantly colder than
the other members.
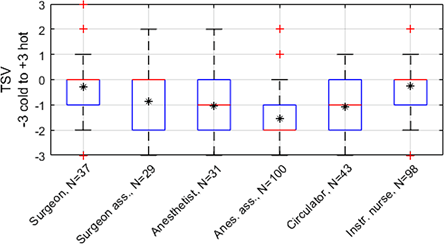
Figure 3.
Survey results – uniform thermal comfort. The TSV (Thermal Sensation Vote) is
an index on the 7-point thermal sensation scale ranging from -3 (cold) to +3
(hot) with 0 as neutral.
In case of
non-uniform thermal comfort, the differences are less pronounced (Figure 4).
In general, hands and arms are often perceived as cold as a result of draught.
The surgeon generally has fewer complaints. The anesthesiology
assistant has significantly more complaints in comparison to the other members
of the surgical team.
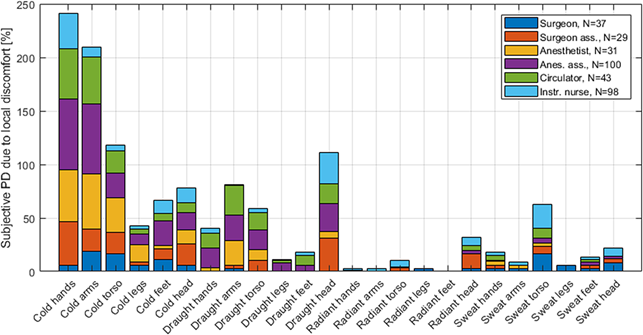
Figure 4.
Survey results – non-uniform thermal comfort. The surgical staff members are
subdivided per function and were able to give multiple answers regarding local
discomfort. Therefore, the total percentage of dissatisfied people can exceed
100%.
The effect
of the type of ventilation system on the assessment of the general thermal
sensation and acceptance does not show any significant differences. Every type
of ventilation system seems to have its own specific complaints with respect to
local discomfort. But these differences are not significant based on the
available data. In the survey three different type of ventilation systems were
compared: 1T plenum (N=72), 2T plenum (N=165) and Opragon (N=24).
Comparing
the subjective data with theory, an assessment can be made of the extent to
which the existing ISO7730 standard is applicable to the operating theatre (Figure 5).
It is assumed that the outcome for the TAV (Thermal Acceptance Vote) is
representative for the degree of dissatisfaction (PD: Percentage of Dissatisfied
people).
|
|
|
Figure 5. Subjective perception versus the percentage of
dissatisfied persons [PD] and a comparison with the theory (A: all members of
the surgical team together; B: subdivided by function) [3]. |
The results
show that in case of the operating theatre the theory underestimates the number
of satisfied people. The subjective results do show the same trend as the
theoretical model. The individual results per team member show that there are
clear differences in thermal perception (Figure 5B).
Preferences are both on the cool and on the warm side. This clearly shows the
complexity of the problem in the design of such systems.
Objective data – The comparison of the objective data
(measurements) for the different systems (at an average set point temperature
of 20°C) shows that the PMV (Predicted Mean Vote) ends up on the cold side (≈−1)
of the thermal sensation scale. The systems that are studied show little
differences. The variation is also comparable for each position where
measurements took place (see Figure 1C). The anesthesiology assistant (position 2 and 4) has the
worst thermal sensation (lowest PMV value). For the instrument nurse (position 3)
the situation is somewhat better based on the PMV value. With regard to local
discomfort, especially draught is a problem (see Figure 6).
The positions under the ventilation system are most critical, although at
Hospital B the differences with the other positions are not significant. The
vertical temperature gradient and floor temperature pose little or no problems.
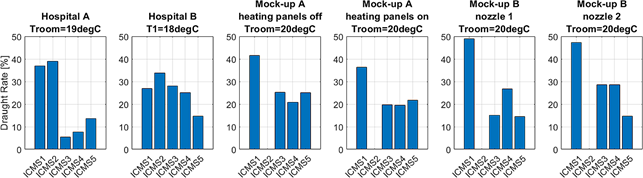
Figure 6.
Theoretical percentage of draft complaints (PD) based on objective measurements
for the different positions in an operating theatre (see Figure 3) with
different types of systems and conditions (For Opragon and Halton it was not
possible to measure at position 2 [ICMS2] due to a non-functioning
sensor).
Comparing
the measurements results for the draught rate (DR) with the subjective (survey)
data, it is noticed that the surgeon has few draught complaints (position ICMS1),
while the measured data indicates otherwise. Referring to the survey results,
the Opragon system also shows more draught complaints
compared to the other systems (DROpragon= 46% compared to DRUDF_T1 = 36% and DRUDF_T2 =
34%). This is not reflected in the measurement results (DROpragon
= 25% compared to DRUDF_T2 = 24%).
The results
provide interesting insights into the current situation in operating theatres
in the Netherlands with regard to thermal comfort of the surgical team. These
results show that improvement is possible and desirable for better thermal
conditions. Although no statement can be made about the effect on work
performance, it may be suspected that in line with what is known about the
office environment [7], this performance is affected by thermal comfort. In
this case, work performance must be translated in the quality of the execution
of the surgery. This could be one of the reasons why, in theory, more efficient
systems (based on air quality) perform less than expected [8].
The results
of the survey indicate that there are fewer complaints than theory suggests
based on the average thermal sensation (PMV). This is not in line with the
hypothesis that people would be more critical since the adaption possibilities
in an operating theatre are limited. It may be assumed that the focus on the
patient makes the own thermal comfort a bit more subordinate. If that is the
case, it is questionable whether that is a good choice. However, the PMV model
has been developed especially for an office environment [4]. At individual
level (member of the surgical team) the agreements are better. This is in line
with the results from Van Gaever et al. [2].
Draught
perception is experienced differently in an operating theatre than theory
indicates. The measurements show high percentages of draught complaints,
especially underneath the plenum. The subjective data show, however, that the
surgeon has almost no draught complaints. Contrary, other members clearly show
more draught complaints than the measurements (and therefore theory) suggest.
The different systems show some differences in the evaluation of draught, but
generally reveal the same pattern with higher values underneath the plenum.
The
limitations in the research must also be mentioned. Clothing and metabolism
have an important effect on the PMV values. No specific data were available for
surgical staff and, on top of that, the survey showed that there were clear
differences in clothing levels between the different hospitals. Additionally, a
standard operating theatre with a standard setup has been assumed during the
research. In combination with information from literature, clothing insulation
(Icl)
and metabolism (M) have been set for the different
members of the surgical staff (Icl = 0.5 – 0.69 clo;
M = 1.5 – 1.6 W/m²). This may not be applicable
for specific surgeries. Furthermore, it is assumed that some survey questions
were not interpreted correctly in a few cases. If misinterpretation was assumed
based on the response to the other questions, the results were excluded from
the analysis.
The
measurements could not be performed simultaneously with an actual surgery due
to hygienic reasons. The location of heat sources and settings of the operating
theatre were somewhat limited by the applicable rules. Besides, it was not
feasible in this study due to limitations of the reserved research time, to
perform measurements for all three use situations in all variants. For those
cases where this was possible, measurement situation 2 (static) and situation 3
(dynamic) led to similar conclusions in terms of thermal comfort.
This
research shows that the thermal comfort in operating theatres for the members
of a surgical team is perceived as not optimal. The distinction in perceived
satisfaction for the different members is also evident. Application of the
theoretical PMV and DR models needs further attention when applied for
operating theatres. Future research may focus on this issue.
The direct
effect of thermal (dis)comfort on the outcomes of a surgery is unknown since
specific information for the operating theatre is missing. However, it seems
appropriate to give this aspect a more prominent role in the development of
ventilation systems for operating theatres than has been the case until now.
Disconnecting the air quality issue about the thermal issue seems to be an
interesting option in order to find an optimal combination about both aspects
[9].
Possible
improvements can also be found in clothing adjustments. It is expected that the
possibility of covering arms, hands and neck against cold and draught will
contribute positively to the thermal sensation of the individual staff members.
In all cases, the most important goal remains the health and safety of the
patient. In an operating theatre, there is little discussion about this.
This
investigation would not have been possible without the hospitals and the
operating staff who cooperated in this investigation. This also applies to Avidicare, Optimus and Halton, who made their facilities
available for carrying out measurements. Finally, a word of thanks to the BPS
laboratory of the TU/e, and especially Wout van Bommel, for preparing the measurements and the associated
measuring equipment.
The whole
report can be found here: https://pure.tue.nl/ws/portalfiles/portal/108242086/Jacobs_0815645.pdf
[1] Gormley, T., Markel, T.A.,
Jones, H.W., Wagner, J., Greeley, D., Clarke, J.H., Abkowitz, M., Ostojic, J. (2017). Methodology for
analysing environmental quality indicators in a dynamic operating room
environment. American Journal of Infection Control 45, pp. 354-359.
[2] Van
Gaever, R., Jacobs, V.A., Diltoer,
M., Peeters, L., Vanlanduit,
S. Thermal comfort of the surgical staff in the operating room. Building and
Environment 81, pp. 37-41. 2014.
[3] Sadrizadeh S, Loomans MGLC. Thermal comfort in hospital
and healthcare facilities: a literature review. In IAQVAC 2016, the 9th
International Conference on Indoor Air Quality Ventilation & Energy Conservation
in Buildings, 23-26 October 2016, Seoul, South Korea. s.l.:
s.n.2016. p. 1-12. 1049. 2016.
[4] International Organization
for Standardization (ISO). NEN-EN-ISO 7730: 2005. Ergonomics of the thermal
environment – Analytical determination and interpretation of thermal comfort
using calculation of the PMV and PPD indices and local thermal comfort
criteria. 2005.
[5] Ottenheijm, E.M.M., Loomans,
M.G.L.C., Kort, H.S.M. & Trip, A. Thermal comfort
assessment in a Dutch hospital setting – model applicability. Proceedings of
the 14th International Conference on Indoor Air Quality and Climate. Gent, België. 2016.
[6] Jacobs, I.M. Thermal comfort of surgical
staff in operating rooms with different types of ventilation systems A study
towards design solutions for optimized thermal conditions. Master graduation
thesis. Eindhoven University of Technology. Department of the Built
Environment. Mastertrack Building Physics and Services.
Eindhoven. pp. 148. 2018.
[7] REHVA. Indoor climate and
productivity in offices. Guidebook No.6. Federation of European Heating,
Ventilation Associations. 2006.
[8] Allegranzi, B., Zayed, B. Bischoff, P. et al. New WHO recommendations on
intraoperative and postoperative measures for surgical site infection
prevention: an evidence-based global perspective. Lancet Infectectious
Diseases. Published online November 2nd 2016.
(http://dx.doi.org/10.1016/S1473-3099(16)30402-9).
[9] Loomans, M. G. L. C., de Visser, I. M., Loogman, J. G. H., Kort, H. S. M.
Alternative ventilation system for operating theaters:
parameter study and full-scale assessment of the performance of a local
ventilation system. Building and Environment. 102, pp. 26-38. 2016.
Follow us on social media accounts to stay up to date with REHVA actualities
0