Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities

|
|
|
|
André Schlott | Thomas Hutsch | Eileen Sauer | Jens Wetschky |
Fraunhofer Institute for Manufacturing Technology and Advanced Materials IFAM, Branch Lab Dresden, Dresden, Germanyandre.schlott@ifam-dd.fraunhofer.de | Fraunhofer Institute for Manufacturing Technology and Advanced Materials IFAM, Branch Lab Dresden, Dresden, Germany | Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB, Stuttgart, Germany | Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB, Stuttgart, Germany |
|
|
|
|
Jana Hessel | Susanne Bailer | John Laubert | Stefan Lösch |
Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB, Stuttgart, Germany | Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB, Stuttgart, Germany | Fraunhofer Institute for Manufacturing Technology and Advanced Materials IFAM, Bremen, Germany | Fraunhofer Institute for Manufacturing Technology and Advanced Materials IFAM, Bremen, Germany |
Aerosols containing viruses can accumulate indoors and lead to superspreading events [1]. Therefore, slowing down the rate of spread is an essential goal in order to control the pandemic spread of viruses (e.g. SARS-CoV-2) and other pathogens. That can be achieved by interrupting transmission chains.
Researchers all over the world work on air purification technologies. Possible air purifying technologies include filtration with HEPA filters, where the viruses are removed from the air volume. This is a common approach to reduce contamination in the surrounding air. With light in UV-C spectrum (200 to 280 nm), viruses are deactivated through critical damage to the genomic system of the microorganism by absorbing photons [2, 3]. With UV light, surfaces, e.g. door knobs, are sterilized [4]. To clean air volumes, an upper-room mounting of UV lights is possible [5]. Additionally, UV lights are installed in HVAC channels. A third method is the plasma air cleaning, which uses high-voltage electrodes to create ions in the air [6].
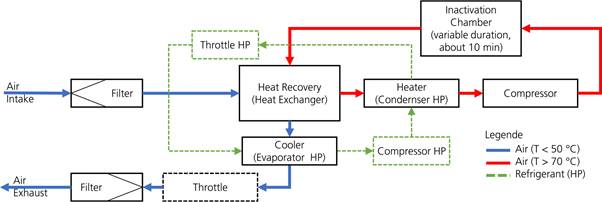
Figure 1. Flow chart of the sterilization process.
The developed apparatus ‘Virus-Grill’ reduces the probability of droplet infection by inactivating viruses. This inactivation is achieved by heating the viruses beyond their temperature sensitivity. (e.g. 70°C), the virus proteins, especially the surface proteins needed to dock to receptor molecules on the host cell membranes, are denaturized.
If this targeted process is carried out continuously, it can be used as a kind of "virus sink". In order to return the inactivated air to the room, the air must be cooled down to nearly room temperature. The use of a heat pump enables efficient temperature control within the apparatus. The interaction of the components is ensured by a regulation and control software.
The aim was to construct and build up a test rig for the proof of the inactivation of viruses using a safety workbench. The developed principle itself can be integrated into climatization systems for closed volumes like rooms (bureau; waiting rooms; class rooms; passenger areas in aircrafts, hotels and ships).
The concept of the ‘Virus-Grill’ is that a partial quantity is extracted from a closed volume of air by the compressor and is specifically exposed to a higher temperature (e.g. more than 70°C) in the apparatus for at defined dwell time (e.g. 10 minutes in a dwell chamber). Before the air reaches this chamber, it is heated in three steps as shown in Figure 1. The heating steps one and two utilize the already treated and still hot air. While the first step is a passive heat recovery system, the second step uses an active heat pump to heat the air. The final heating step is the compressor itself, where the air reaches the temperature needed during compression. After that, the compressed air is stored in a heated chamber to inactivate the viruses. The viruses will stay in the treated air but because they are not infectious anymore, the air is considered inactivated / purified.
After releasing the sterilized air from the chamber, it goes through the heat recovery and the evaporator of the heat pump to reduce its temperature. Before leaving the apparatus, a throttle reduces the pressure of the air. Therefore, the air leaves the ‘Virus-Grill’ apparatus at ambient pressure and almost at ambient temperature.
The set-up was done considering the planned tests with surrogate viruses in a safety workbench to characterise the effectiveness of the ‘Virus-Grill’. Because of the limited space in the workbench, the test rig had to adhere to certain dimensions. Also, the required air volume of the aerosol generator and available electrical connection were considered at the design process of the test rig.
Figure 2 shows the set-up of the ‘Virus-Grill’ during the trials for the proof of efficacy.
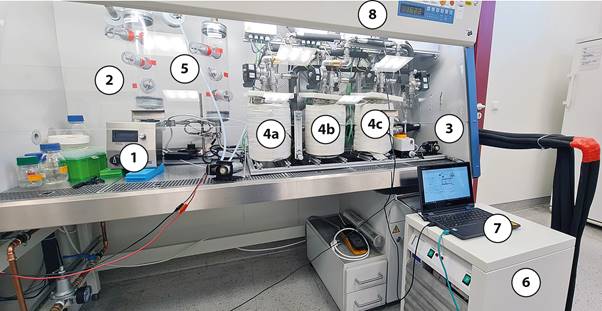
Figure 2. Prototype of the ‘Virus-Grill’ in the sterile bench environment to characterise the efficacy in terms of inactivation of aerosol-borne viruses. (1) aerosol generator, (2) virus chamber, (3) compressor, (4a-4c) holding chambers, (5) clean chamber, (6) heat pump, (7) measuring computer with control software, (8) safety workbench (sterile bench).
The individual components play a special role in this process, the sum of which can achieve effective inactivation. The compressor works according to the principle of a piston compressor. This causes pressure (change) and temperature to act for a short time. In addition, the pressure-resistant dwell chambers (here 3 bar) are tempered to a certain temperature by an external heater. In order to use energy more efficiently, the heat pump supports the heat recovery unit used. The developed system of solenoid valves enables almost continuous operation through appropriate control. The question of effectiveness was addressed as a complete unit as well as in partial component tests.
The ‘Virus-Grill’ control includes the collection and processing of numerous temperature and pressure sensor data and adjustable process parameters. Valves and compressor are controlled by control electronics containing market available and self-developed components. The ‘Virus-Grill’ is monitored by 16 temperature sensors (PT1000) and 16 pressure transmitters, whose data are processed by the controller. Switching operations on solenoid valves and air compressors as well as power control of the heat pump components are made possible by means of a Mosfet driver circuit and an external power supply. The control of the chamber heating is realised via standardised interfaces.
A microcontroller board is used as the central element of the control system, which has sufficient computing power and supports all necessary connections. The necessary firmware was programmed in C++ and processes the measurement data, interprets process parameters and gives corresponding control signals. A wireless LAN access point including a webserver enables the user to interact with the ‘Virus-Grill’.
A control software developed in C# establishes the necessary connection and displays the measurement data using a circuit diagram of the ‘Virus-Grill’ (Figure 3). The measurement data are stored in parallel for later evaluation. It is also possible to adjust the process parameters of the ‘Virus-Grill’.
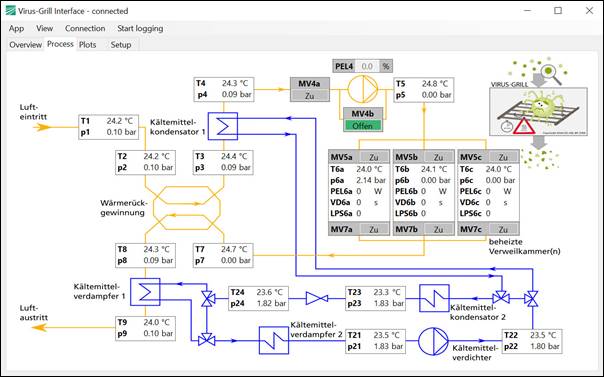
Figure 3. GUI of the control software.
In order to take suitable samples, aerosol samples must be collected from a closed system, such as the virus and clean chamber, without manipulating the atmosphere in the system or allowing air contaminated with viruses to escape. Therefore, a small airlock for swabs was developed and four polycarbonate 3D printed components were created for each airlock, which were assembled with UV-resistant adhesive.
The construction is shown in Figure 4. The three-part airlock consists of a handpiece, a piston insert and the actual airlock chamber as well as the piston. The handpiece serves as a carrier/holder for the swab and at the same time as the "outer sluice gate". The piston insert combines inner and outer sluice gate including the necessary piston seals. The piston itself determines the volume of air exchanged when opening and closing the airlock.
The greatest difficulty in the CAD-supported development was the sealing ability of the piston rings. The tubes used, made of special solvent-resistant and UV-permeable acrylic glass, showed strong geometric tolerances, so that commercially available sealing solutions with rubber rings and lubricants and sealants did not achieve sufficient sealing. Therefore, piston sealing rings made of flexible filament were developed and manufactured by means of 3D printing, with which tolerances could be compensated and a sufficient seal achieved at both sluice gates. These are shown in red in Figure 4. Smooth sliding of the piston insert was also ensured.
To close the sluice gates securely, neodymium magnets are used to magnetically attract a metal ring on the handpiece itself or on the outer end of the piston, depending on the position of the handpiece. These metal rings required precise manufacturing in order to minimise the gap between the magnets and the metal ring so that the neodymium magnets can generate a sufficiently large magnetic attraction force.

Figure 4. Three-part airlock for sampling (above: Handpiece/swab holder; middle: piston insert with sealing ring; bottom: printed components)
The current and still ongoing pandemic situation regarding SARS-CoV-2 requires standardised methods for the detection and analysis of airborne viruses in the form of aerosol. Since SARS-CoV-2 is classified as a biosafety level 3 virus, the number of laboratories that can culture and analyse infectious viruses is severely limited and the experiments require a high level of security measures for containment. For this reason, the bacteriophage Phi6 was established as a surrogate virus. Phi6 shows a high degree of similarity to SARS-CoV-2 in particle size, external structure, and the type of genome. In contrast to other surrogate viruses, Phi6 is a bacteriophage that only infects bacteria and poses no danger to humans, animals or plants. In order to assess the effectiveness of disinfection measures, two parameters were applied. i) The number of viral genomes that accounts for all viruses whether dead or alive, was determined by the molecular biological method of qPCR. ii) The viral activity or infectivity that accounts the number of infectious viruses was determined by the plaque assay.
The bacteriophage Phi6 was used as surrogate virus for the evaluation of the ‘Virus-Grill’. Phi6 was propagated using its host bacterium Pseudomonas syringae. Stock solutions of Phi6 and P. syringae were kindly provided by Prof. Dr. Martin Hessling and Dr. Petra Vatter (Technische Hochschule Ulm). For propagation of the surrogate virus, P. syringae was cultivated overnight in tryptic soy broth (TSB) at 25°C and 170 rpm. Bacterial culture was subcultivated in fresh TSB for starter culture. At an optical density of 0.3, Phi6 was added 1:10 followed by incubation to an optical density of 0.08. To obtain pure phage lysate, the culture was centrifuged to pellet the bacteria, and supernatant was filtered through a 0.45 µm filter (Fisher Scientific).
For all experiments performed, Phi6 lysate was rebuffered in water. The titer of the obtained Phi6 stock lysate was determined using a bacterial plaque Assay [7] and stored at 4°C until further usage. For the experimental procedures, the stock lysate was adjusted to 1 × 1010 PFU/mL and used for aerosolization.
The individual steps of sampling with this airlock are shown in Figure 5. After inserting the swab into the handpiece, it was mounted in the piston insert. At the same time, the outer airlock is closed. For sampling, the entire piston insert is guided into the interior of the system, exposing the swab to the aerosols. When the piston insert is pulled out, the inner lock closes and the handpiece with the swab can be removed again. The escape of aerosols can thus be reduced to a minimum.
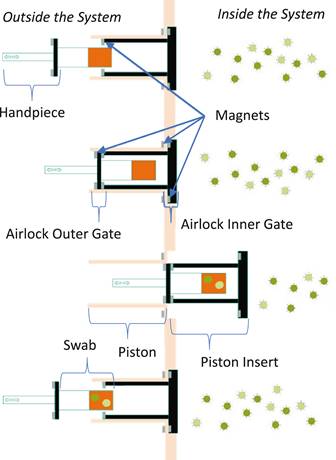
Figure 5. Sampling concept with airlock and swab
For the experimental set-up, a droplet aerosol with an average droplet size of 0.15 µm was generated from a phosphate-buffered saline (PBS) containing Phi6. The aerosol was collected and analysed at three positions before the experimental setup (virus chamber) and after the experimental setup (clean chamber) using swabs moistened in PBS. All samples were analysed for virus activity and total virus count.
Four different experiments were conducted to examine partial components of the ‘Virus-Grill’ and finally the entire test rig. In the first experiment (Exp. 1), the virus-containing aerosol was sucked from the virus chamber into the clean chamber. The pump was behind the clean chamber. This was done to find a baseline of surrogate viruses in the virus chamber and clean chamber with no treatment whatsoever. In the second experiment (Exp. 2), the virus-containing aerosol was pumped from the virus chamber through the pump into the clean chamber. In the third experiment (Exp. 3), the virus-containing aerosol was pumped pressure-free from the virus chamber through the ‘Virus-Grill’ into the clean chamber. Again, the pump was located at the end of / after the clean chamber. And in the fourth experiment (Exp. 4), the virus-containing aerosol was pumped from the virus chamber through the ‘Virus-Grill’, through the pump into the clean chamber at room temperature and 1.5 bar overpressure.
The results of the detection of the virus activity and the determined virus genome count are shown in Figure 6 and Figure 7. It was shown that only in Exp. 1, in which the viruses were sucked directly from one chamber to the other, were active viruses detectable in the clean chamber.
The detected virus genomes in Figure 7 show an increasing reduction of virus genomes when using the pump in Exp. 2, the flow through the ‘Virus-Grill’ in Exp. 3 up to the greatest reduction of virus genomes when operating the ‘Virus-Grill’ at room temperature and a system pressure of 1.5 bar in Exp. 4.
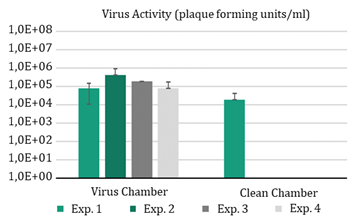
Figure 6. Comparison of virus activity in virus chamber and clean chamber.
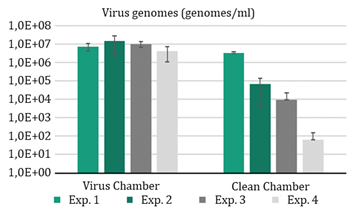
Figure 7. Detected viral genomes in virus chamber and clean chamber The viral genomes detect both inactivated and infectious viruses.
Taken together, it was possible to aerosolise surrogate viruses in the experimental set-up, to transport them from the virus chamber into the clean chamber and to detect them. The use of the pump already leads to complete inactivation of the viruses used. This leads to the hypothesis that continuous inactivation is possible by using compressors based on the principle of the piston compressor for SARS-CoV-2. Furthermore, the use of the ‘Virus-Grill’ was able to reduce the total number of virus genomes.
The efficacy of the ‘Virus-Grill’ was validated with four experiments. Exp. 1 defined a baseline of viruses reaching the clean chamber with no treatment whatsoever. Experiments 2 to 4 tested different ‘Virus-Grill’ configurations. Exp. 2 pulls the virus-containing aerosol only through the piston pump into the clean chamber. In experiments 3 and 4 the contaminated air flows through the complete ‘Virus-Grill’ at ambient pressure and at an elevated pressure of 1.5 bar, respectively. The number of active viruses were reduced below the limit of detection in all three cases. The number of viral genomes in the clean chamber shows that there are inactivated viruses carried through the ‘Virus-Grill’.
This process has very high potential in applications that dispense mechanical filtration. Here, maritime applications and integration into existing ventilation systems are mentioned in particular. The concept can also be adapted in the medical field for the ventilation of patients. Thus, a wide range of flow rates from a few l/min to several m³/min can be addressed through suitable design and scaling of the components.
The presented work was part of the project AVATOR and funded by the Fraunhofer-Society within the Fraunhofer vs. Corona campaign which is gratefully acknowledged.
[1] Miller, S.L., et al., Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event, Indoor Air 31 (2020), p. 314-323, DOI: 10.1111/ina.12751.
[2] Raeiszadeh, M., et.al., A Critical Review on Ultraviolet Disinfection Systems against COVID-19 Outbreak: Applicability, Validation, and Safety Considerations, ACS Photonics 2020, 7, 11, 2941–2951, DOI: 10.1021/acsphotonics.0c01245.
[3] Fukui, T. et.al., Exploratory clinical trial on the safety and bactericidal effect of 222-nm ultraviolet C irradiation in healthy humans, PLoS ONE 15(8): e0235948., DOI: 10.1371/journal.pone.0235948.
[4] Storm, N., et al. Rapid and complete inactivation of SARS-CoV-2 by ultraviolet-C irradiation. Sci Rep 10, 22421 (2020). DOI: 10.1038/s41598-020-79600-8.
[5] Beggs C. B., et.al., Upper-room ultraviolet air disinfection might help to reduce COVID-19 transmission in buildings: a feasibility study, PeerJ 8:e10196, DOI: 10.7717/peerj.10196.
[6] Fennelly M, et al. Effectiveness of a plasma treatment device on microbial air quality in a hospital ward, monitored by culture, J Hosp Infect. 2021; 108:109-112. doi:10.1016/j.jhin.2020.11.006.
[7] Kropinski, A.M., et al., Enumeration of bacteriophages by double agar overlay plaque assay, in Bacteriophages. 2009, Springer. p. 69-76.
Full article: https://proceedings.open.tudelft.nl/clima2022/article/view/214
The datasets generated and analysed during the current study are not available because of the ongoing validation and up-scaling process but the authors will make every reasonable effort to publish them in the near future.
Follow us on social media accounts to stay up to date with REHVA actualities
0