Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
Pawel Wargocki |
International Centre for Indoor Environment and EnergyDepartment of Civil Engineering (DTU BYG)Technical University of Denmarkpaw@byg.dtu.dk |
Ventilation with outdoor air has always been our “ally” in reducing the concentration of air pollutants indoors and thus in mitigating discomfort and health risks, including the risk of infection from airborne pathogens. In the past, when buildings were less airtight, ventilation was obtained by infiltration through the building envelope, shafts, or operable windows (adventitious ventilation); today, it is usually achieved by specially designed systems that not always but predominantly are mechanical. The positive effect of ventilating rooms with outdoor air is only obtained if the outdoor is clean and less polluted than indoors, which is the usual assumption when designing ventilation and is frequently the case. Simulation of indoor exposures to outdoor air pollutants brought in by ventilation imply, however, that increasing ventilation without proper filtration and air cleaning will considerably increase the burden of disease caused by these pollutants [1]. These results underline the importance of ensuring that clean outdoor air is supplied indoors instead of assuming that outdoor air is clean. The few published studies showing that increasing outdoor air resulted in an increased risk of health seem to have made this flawed assumption [2].
Increasing building ventilation, which should be understood in this article as an increased outdoor air supply rate, has otherwise been documented and summarized in many reviews [3,4,5,6] to improve indoor air quality and benefit health, comfort, office work, and schoolwork. The positive effect of ventilation was demonstrated in the classical studies of Yaglou et al. [7], where ventilation requirements to control body odour were determined; their results were verified later in experiments performed in Denmark [8], USA [9] and Japan [10]; in each of these experiments, increasing ventilation improved indoor air quality by reducing odour intensity or the percentage dissatisfied with the air quality as estimated from subjective ratings of the acceptability of air quality. Evaluations of the air quality were made upon entering the space. Other experiments, with occupants remaining indoors until they were adapted to the indoor air quality showed no effect of increased ventilation on ratings of air quality when the air pollution source was body odour [11], but did show an improvement in perceived air quality when the air was polluted by emissions from building materials [12]. Today, these results form the basis for the ventilation requirements prescribed by ASHRAE Standard 62.1 [13] and EN 16798-1 [38]. Increased ventilation was also shown in many studies to reduce both the prevalence and intensity of non-clinical acute health symptoms known either as Sick Building Syndrome (SBS) symptoms [14] or building-related (BRS) symptoms [15] independent of the recall time of these symptoms. The risk of increased symptoms, expressed as the probability (odds) of symptoms being reported as a consequence of reduced ventilation, was estimated, i.a., by Sundell et al. [16] and Fisk et al. [17]. Finally, increased ventilation was shown to improve the performance of office work by adults [18] and of schoolwork (and hence learning) by children [19]. Other studies showed that improved ventilation could be expected to reduce short-term absence rates for both adults [20] and children [21,22]. Ventilation can also reduce the transmission of infectious diseases [23]. Although some control of the risk associated with these pathogens can be obtained by filtering the air with high-efficiency filters, by disinfection of air using, for example, UV-C, to achieve virus-free air, good ventilation with clean outdoor air is also essential. However, the epidemiological data does not provide clear evidence on the required ventilation rates that should be provided in buildings to reduce the risk of infection with airborne pathogens r [24]. Still, estimations using the Well’s-Riley model document this effect [25], as well some studies analysing outbreaks related to SARS-CoV-2 [26].
In many of the above studies, carbon dioxide (CO₂) was used as a proxy for ventilation [27,28]: The ventilation rate was not measured directly but was calculated using measured concentrations of CO₂ and assuming the metabolic rate of building occupants and good mixing of air within a space. Relationships were also created between the concentration of CO₂ and different outcomes, including health [29] and cognitive performance [19]. Rudnick et al. [25] developed a CO₂-based risk equation to estimate the risk of indoor transmission of infection by the airborne route. These results do not imply that CO₂ is a causative factor, although they are sometimes interpreted this way. CO₂ is simply a marker of ventilation efficiency (when occupants are present). Some studies published recently have shown that pure CO₂ can reduce some aspects of cognitive performance; specifically, decision-making in complex and time-stressed tasks, at levels as low as 1,000 to 2,500 ppm [30,31], the performance of pilots at 1,500 ppm [32], and some have even claimed that pure CO₂ can affect office-type work such as proof-reading at levels as low as 3,000 ppm [33], although other studies were unable to confirm these results [34,35]. The comprehensive reviews by Fisk et al. [36] and Du et al. [37] show the inconsistency of the results concerning the effects of pure CO₂ on cognitive performance at levels typically occurring indoors, i.e., below its permissible occupational limit of 5,000 ppm. They concluded that it is more likely that no effects are to be expected. They also show that no effects on health or comfort are to be expected at these levels. Thus, attributing the negative effects on building occupants only to CO₂ levels is incorrect. Increasing ventilation will, of course, reduce the concentration of CO₂ that has been emitted by building occupants (if present) and also the concentrations of pollutants emitted from many other sources of pollution indoors, including humans and their activities, building, and furnishing, used filters as well as smoking (if occurring) and combustion. These emissions are mainly responsible for the effects observed in the studies described above and should be the main focus rather than CO₂.
Despite the above evidence, some central questions about ventilation are still not completely answered. Among others, which outcome shall be used to prescribe ventilation requirements in buildings, and consequently, how much ventilation is necessary? This problem is nicely exemplified in Figure 1 showing how ventilation rates changed over time. The difficulty to set ventilation requirements was also the case when one of the first ventilation guidelines were proposed by the Chicago Commission on Ventilation in 1914 and in 1923 re-confirmed by the New York State Commission on Ventilation. No ventilation requirements were proposed back then, although setting ventilation was the main purpose of these committees. There were only general recommendations regarding the methods on how to achieve ventilation. Window-ventilated rooms with natural draft were the preferred method of ventilation proposed in these documents, but ventilation was not recommended to avoid ill health, but to avoid over-heating. Temperatures of 15–19°C in window-ventilated rooms were observed to cause the lowest prevalence of respiratory illnesses, so the resulting guidelines recommended 20°C with proper control of relative humidity for living rooms. CO₂ was not recognized as a harmful agent. Ventilation was basically required to control humidity, and this would be impossible if 100% of the air was recirculated.
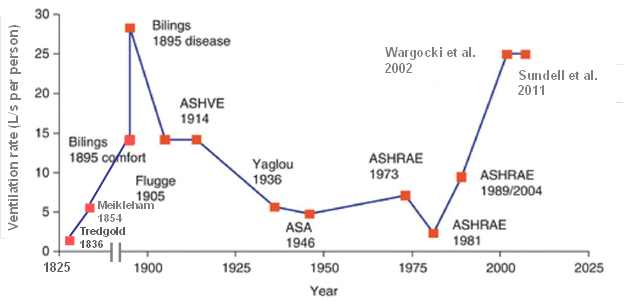
Figure 1. Ventilation requirements in buildings – historical perspective (adapted from Nielsen and Li). [64]
Today, most of the major standards define ventilation requirements based on the resulting air quality as building occupants perceive it. They consider pollutants emitted by both humans and building materials, and stipulate the air quality and ventilation requirements based on the percentage of visitors dissatisfied with the air quality upon entering the space [38] or on the acceptability for both visitors and occupants [13]. These standards implicitly assume a connection between fulfilling comfort requirements and fulfilling the requirements for health, assuming that if the former is reached, the latter will be ensured as well. Brelih [39] and Dimitroulopoulou [40] showed that ventilation in numerous buildings does not comply with the requirements in the standards, while Asikainen et al. [41,42] showed that substandard ventilation in homes will result in an increased burden of disease, which is providing some support to the above assumption on health effects. It is still pertinent to ask whether other criteria than sensory discomfort should be used to determine ventilation requirements in buildings or whether the current requirements are sufficiently able to reduce the risks related to exposures that are not affected by air quality as perceived by building occupants.
The reasons given for the need for ventilation changed over time (Boxes 1 and 2). Figure 1 shows that ventilation requirements changed too. It shows that the requirements are nearly "everywhere" on the figure, and they differ by an order of magnitude. Tredgold proposed the lowest ventilation in 1836; he suggested that the minimum ventilation rates in mines should satisfy the physiological needs of a miner. It was set at 1.7 ℓ/s per person, of which 0.2 ℓ/s was for purging CO₂ from the lungs, 1.4 ℓ/s for removing the moisture produced by the body, and 0.1 ℓ/s for keeping a candle burning. One of the highest rates was proposed 170 years later using the results of two reviews of peer-reviewed literature on ventilation and its effect on man showing that at 25 ℓ/s per person, no negative effects on health symptoms and the performance of office work are to be expected [4,43]. Billings proposed the highest ventilation rate in buildings in 1893 to reduce the risk of spread of tuberculosis and recommended between 30 and 60 cfm/person (14–28.5 ℓ/s per person).
Box 1. Ventilation, some historical developmentsIn ancient Egypt ventilation was deemed essential for stone carvers, to avoid exposure to particles and dust generated during this process. Hippocrates (460-377 B.C.) described the adverse effects of polluted air in crowded cities and mines. During Roman times (1st B.C.), Sergius Orata developed hypocausts as an under-floor heating system capable of distributing heat uniformly in a house and, most importantly, avoiding combustion indoors and, subsequently, harmful exposures. In the case of open fires indoors, a minimum ratio of window to floor area was set, and parchment above the window was required to assure the supply of air due to infiltration. In Venetian times, roof windows were developed and Leonardo da Vinci claimed that no animal could live in an atmosphere where a flame does not burn, and that dust can cause damage to health, implying a need for ventilation. In the 17th Century, Wargentin expressed the common knowledge of this time that expired air was unfit for breathing until refreshed. In the same Century, Gauger quoting Cardinal Melchior de Polignac, remarked that it is not warmth but inequality of temperature and want of ventilation that causes maladies. In 1756 Holwell described an accident in the Black Hole of Calcutta, a small dungeon where prisoners and soldiers were kept overnight in poor conditions, in which 125 out of 146 died due to suffocation. During the Crimean War (1853-1855), there was a faster spread of diseases among wounded soldiers in poorly ventilated hospitals. A higher morbidity and mortality were observed in overcrowded, poorly ventilated rooms. Immediately after, Florence Nightingale stated that the air the patient breathes should be as pure as the external air, without chilling him. The importance of ventilation in small room volumes, to avoid the death of the occupants, was emphasized by Beeton in 1861 and Baer in 1882. A few years later, Reid expressed the view that along with mental anxiety and defective nutriment, defective ventilation should be considered as one of the evil enemies of the human race. Griscom expressed a similar view in 1850 and acknowledged that deficient ventilation is fatal as it leads to the spread of tuberculosis and other diseases. An effective treatment of tuberculosis using country fresh air was then achieved by Trudeau, who opened the Adirondack Cottage Sanatorium in 1873. In the early 20th century, Winslow and Palmer suggested that poorly-ventilated rooms do not create much discomfort but do result in loss of appetite. Later, Winslow and Herrington obtained a similar result - loss of appetite for food when heating dust from a vacuum cleaner. |
Box 2. Some theories underlying the need for ventilation through historyThe miasma theory prevailed until XVIII–XIX Century, attributing cholera, Chlamydia, and the Black Death to a noxious form of “bad air.” The germ theory of disease later displaced it after germs were discovered in the XIX Century. In the early XVII Century breathing was believed to result in a cool heart. In the same Century, Mayow attributed the effects observed to igneo–aerial particles that cause the demise of animals. One Century later, in 1775, Lavoisier identified two gases in the air and attributed the effects of igneo-aerial particles to carbon dioxide (CO2) and air stuffiness. The theory that CO2 is a dominant cause of the physiological effects of bad air remained dominant for nearly 100 years, although it was acknowledged that other factors could also contribute to the effects observed. It prevailed until Pettenkofer in the 1800s, demonstrated that it is neither the deficiency of oxygen (O2) nor excess of CO2 but the presence or lack of biological pollutants (from humans) which are responsible for vitiation of indoor air. In 1872 Pettenkofer and Saeltzer suggested CO2 to be a surrogate for vitiated air, an indicator of the presence of deleterious substances of unknown origin. In 1887–1889 Brown-Sequard and d’Arsonval suggested that anthropotoxin (the toxic effluvia - toxic substances in exhaled air) was responsible for the effects reported through history when there was a lack of ventilation. Organic matter from lungs and skin had also been proposed as poisonous by many others before the anthropotoxin theory. The theory was rejected by many experiments performed later by Haldane and Smith in 1892–93, Billings in 1895, and Hill in 1913. They could not confirm that a condensate of expired air could kill animals, as Brown-Sequard claimed. The anthropotoxin theory was then superseded by an idea proposed by Billings in 1893, suggesting that the purpose of ventilation is to dilute contagions emitted by humans, thus reducing the spread of infectious diseases. A large body of research in the early XX Century, among others by Billings, Flugge, Benedict & Millner, and Hill, showed that lack of ventilation causes discomfort exemplified by unpleasant body odours and raised temperature. At the same time, no negative physiological effects could be observed even at CO2 levels as high as 1–1.5% (10,000 to 15,000 ppm). Lack of ventilation was consequently associated with raised temperature and discomfort. Since studies of Lemberg and Yaglou in the 1930s of the XX century, ventilation has been required to merely keep body odours at an acceptable level, defined to be at a moderate level. In the 1980–1990s, it was also acknowledged that in addition to the body odours emitted by humans, other sources of pollution indoors determine ventilation requirements. However, the general principle of providing ventilation to reduce discomfort by achieving acceptable air quality as perceived by humans was not changed. Ventilation was merely a question of comfort, not health. |
Figure 1 sends several messages. One of them is that it is difficult to define one ventilation requirement that will satisfy all demands and conditions. The reason is quite simple: different approaches were used to define ventilation requirements, different sources were controlled, and different outcomes were managed. If comfort (sensory perception of indoor air quality) is a design parameter and the target is 20% dissatisfied (80% acceptability) and humans are the major source of pollution, the ventilation rate would be about 10 ℓ/s per person as reflected in the current ventilation standards; this supports the widely accepted CO₂ concentration of 0.1% (1,000 ppm) proposed by Pettenkofer [44]. However, if health is considered, the rates required can be much higher and as high as 28.5 ℓ/s per person, as proposed by Billings. The question then is whether we can propose a ventilation rate that will satisfy all needs and criteria? In other words, can we develop a consistent framework for setting ventilation requirements instead of changing these requirements depending on the current contextual needs, assumptions made, and criteria defined? The answer seems to be affirmative, considering that an example of such a framework for ventilation requirements based on health criteria was proposed by the HealthVent project [45].
Setting ventilation requirements is only part of the problem. Scientific and technical literature shows that the design, operation, and maintenance of systems providing the air for ventilation have not always been adequate, resulting in the ventilation systems themselves becoming a strong source of pollution that can increase exposures and consequently increase health risks (e.g., [15,46,65]). The list of reported problems is long. The most common faults include insufficient air inlet size causing a loss of pressure, missing condensate drains for in-ground air heat exchangers and/or ventilation devices, no insulation of ducts conveying cold air (so condensate is formed), poor maintenance of filters, low class of filtration, inaccessible and dirty filters seldom changed for new ones, missing sound attenuators, improper cross-sections of ducts causing the air velocity to be too high or too low, inappropriate material of pipes (flexible tubes), improper location of main air intakes and exhausts, too short distances between air intakes and exhausts, supply and exhaust air openings that cause ventilation to short-circuit, partially or fully blocked (covered) air terminals. These problems have been observed irrespective of building type, and guidelines to deal with them are needed; an example of such a guideline that was developed by the HealthVent project is shown in Box 3.
Box 3. Tentative guidelines for the design, operation, and maintenance of systems used to supply air for ventilation (from the HealthVent project)* The systems should meet ventilation requirements from the start and throughout the entire lifetime of the building. * Low-emitting, certified and durable materials should be used in any system used for ventilation. Emission from fibrous materials should be reduced to a minimum. * Systems used for ventilation should be kept clean throughout the lifetime of a building. They should be cleaned at regular intervals using certified products for wet and dry cleaning that do not elevate exposures. * The performance of mechanical ventilation systems should be verified at the commissioning phase and shall be guaranteed by the suppliers at any time for their entire service life. * Condensation in systems used for ventilation should be minimized to avoid microbial growth. Systems should be properly drained and kept dry. Outdoor air intakes should be protected from rain and snow entrainment. * Air cleaning that emits ozone in systems used for ventilation should be avoided. * Theventilationrateshouldcopewiththeactualneeds and demands and should be based not only on the design parameters but on the actual use and actual occupant requirements. * If a mechanical system is used for ventilation, there should be a contingency plan for ensuring ventilation (e.g., by opening the windows or other measures) in the case of system failure, and in case of blocking and shutting down the systems by occupants or building operators. * All outdoor air intakes, including openings for natural ventilation, should be located so that the direct entrainment of pollutants from nearby sources is minimized. * Ventilation air should be properly distributed within the space to which it is delivered. * The systems used for ventilation shall not become the source of nuisance and annoyance due to noise, vibration or draft at any time from commissioning and throughout its entire lifetime. * The systems used for ventilation should be regularly maintained and inspected during normal operation. The inspections should include at a minimum the same aspects as during commissioning and additionally examination of cleanliness, loading of filters, and the need for re-balancing in case of changing demands. Those obligations shall become the exclusive responsibility of the suppliers of the systems and performed by qualified personnel. * Systems used for ventilation should be designed, operated, and maintained by qualified personnel. The design should address the need for regular maintenance and provide the possibility of override (in case of unusual events). Continuous education programs should be implemented for designers, consultants, and facility managers, which besides technical matters, should address the connection between ventilation and exposures. Operating instructions should always be provided. |
When discussing the criteria that should be used to define ventilation, we have to keep in mind the purpose and role of ventilation in buildings. This is presented in Figure 2. It shows that ventilation is used to reduce exposure to air pollutants, that it is exposure to pollutants that affects human response (not the ventilation), and that ventilation can only be a part of any solution to reduce the exposure. We learn that exposure can also be reduced by other means, including source control, i.e., reducing emissions from products used in buildings or capturing the pollutants at their source, filtration, and air cleaning. Ventilation can be used instead of these solutions, together with them, or once the other solutions are in place and ventilation is the last way of improving indoor air quality, to reduce the risks related to exposures that could not be reduced by other means; in each of these cases, it is, of course, assumed (as pointed out earlier) that the air supplied indoors is clean and this precondition must always be satisfied.
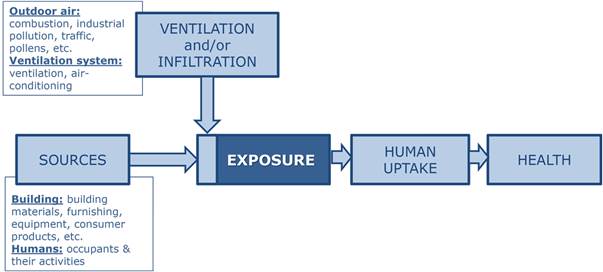
Figure 2. Ventilation is a mediating factor, not a cause.
When ventilation is used as the primary measure to reduce exposure, different literature reviews of ventilation indicate that a ventilation rate of 10 ℓ/s per person [15], 15 ℓ/s per person [29] or 25 ℓ/s per person [4,43] would be necessary to keep indoor air quality high and ensure that health risks and the risk of reduced cognitive performance for building occupants are both kept low; a single study by Federspiel et al. [47] suggests even higher rates might be necessary.
When ventilation is used as a secondary and complementary measure for controlling exposures once other means have been exploited, we need to know the minimum (base) ventilation requirement that must be supplied in buildings when people are present. Different approaches can be used to determine the base ventilation requirement. We have already mentioned the 1.6 ℓ/s per person that Tredgold proposed for miners. Viessman [48] proposed that the minimum ventilation rate that should be ensured to provide oxygen (O₂) for breathing is about 1 cfm/person (ca. 0.5 ℓ/s per person). Following occupational hygiene standards and keeping CO₂ below 5,000 ppm, Sundell [49] proposed 4 ℓ/s per person (with a safety factor of 5); 3 ℓ/s per person was proposed to keep humidity below 45% when only moisture emitted from humans was considered, a rate similar to what was proposed by Viessman [48]. A different approach was used by Carrer et al. [45]. They reviewed the peer-reviewed epidemiological literature and reported the minimum ventilation rates at which no effects for different outcomes were seen. For example, the lowest ventilation rate at which no elevated risk of asthma and allergic symptoms was observed in the published literature was 7 ℓ/s per person [50], while 8 ℓ/s per person was the lowest in the case of acute non-clinical health symptoms in homes [51] and 9 ℓ/s per person in offices [52]. These rates can be considered as the best available tentative and empirically determined estimates of the lowest rates with no observable adverse health effects. For the sake of comparison, if the performance of office work and schoolwork are considered, these rates were higher, about 16-24 ℓ/s per person, and if short-term sick leave is considered, they were 24 ℓ/s per person. Numerous limitations of these rates were indicated by Carrer et al. [6], restricting their generalization: (i) the data were incomparable or difficult to compare; (ii) exposures were improperly characterized; (iii) there were no data on indoor pollution sources, including the maintenance of ventilation systems; (iv) it was assumed that outdoor air was clean (unpolluted); (v) health outcomes were insufficiently characterized and included mainly self-estimated acute symptoms with no data on chronic health effects; (vi) ventilation was inadequately characterized and based often on crude measurements of the ventilation rate; (vii) exposed populations and their sensibility were poorly characterized; and (viii) experimental designs were weak. Considering these limitations, Carrer et al. [45] proposed another ventilation rate as minimum base: 4 ℓ/s person. This rate was assumed to be sufficient to keep the risk for acute health symptoms low, but only if the World Health Organization’s air quality guidelines [53,54,55,56] are met, and the major source of pollution are the occupants.
The risks of infectious diseases were not considered by Carrer et al. One of the reasons was insufficient data. A single study by Sun et al. [57] performed in student dormitory rooms in China that were occupied by more than one student showed that the risk of the self-reported common cold is reduced if ventilation is increased until 5 ℓ/s per person and that any further increase in the ventilation rate will provide only a very small benefit. Generalizations of this result to other buildings and other occupant densities are difficult but a recent study of Li et al. [26] provides some support in which ventilation rates as low as 0.9 ℓ/s per person were suspected to cause the outbreak of COVID-19 in the overcrowded restaurant. Assuming that mild infections cause short-term absence rates, a study by Milton et al. [20] showed that ventilation rates of 24 ℓ/s per person would significantly reduce the risk of absence compared with 12 ℓ/s per person. However, these results were obtained in a cross-sectional study and were not confirmed in intervention studies where the levels of ventilation were about 40–45 ℓ/s per person [58]. Still, another study showed that virus might survive on a filter at ventilation rates as high as about 40 ℓ/s per person, the rate being back-calculated from the measured CO₂ above the outdoor level of 100–200 ppm [59]. With respect to the current COVID-19 pandemic, REHVA recommends ventilation rates that ensure that CO₂ is at or below 800 ppm (i.e., around 10 ℓ/s per person), while ASHRAE recommends that the rates should meet at least the minimum code requirements with improved filtration efficiency [60]. If we consider that during a pandemic, the risk of infection due to airborne pathogens in buildings will be similar to what occurs in hospital wards (patient rooms), it may be inferred that a total ventilation rate corresponding to 6 h⁻¹ would be necessary with high-efficient filtration, of which 2 h⁻¹ would be outdoor air; these are the rates prescribed by ASHRAE Standard 170 for health care facilities [61]. The rate of 6 h⁻¹ would correspond to 17–20 ℓ/s per person in a 100 m² classroom with 25 students or about 5 ℓ/s per m² floor, of which the outdoor component should be at least 30% as in ASHRAE Standard 170 [61]. Hence, this outdoor component would be around 20 ℓ/s per person, which is close to what was found by Milton et al. [20] to reduce absenteeism in practice.
With the evidence described above we can assume that the ventilation rate in buildings can be anywhere between 4 and 25 ℓ/s per person, as also shown in Figure 1.
There are many beliefs regarding ventilation, and many are only partly true. Among the few, it is assumed that more ventilation will always improve indoor air quality, that low ventilation rate always means poor air quality, that it is simple to measure ventilation, that ventilation can be used as a metric predicting human responses, that outdoor air and the air supplied indoors is clean, that ventilation systems are clean, and that the air indoors is fully mixed within the air volume. Irrespective of the different beliefs and opinions about ventilation, and whether or not they are true, we need ventilation in buildings and it must satisfy a number of different criteria. It must be reliable, flexible and well-functioning, adaptable, and responsive to different needs and unusual events. The urgent task of defining ventilation requirements that meet these different criteria must be solved as a high priority and may require out-of-the-box thinking and new advanced solutions for ventilation [62]. In other words, a new paradigm and a framework for defining ventilation in buildings are urgently required.
More research is also required. Current knowledge should be used and supplemented by population- representative measurement campaigns of indoor exposures in all major building types to support improved design. They will fill the gaps in knowledge on the effects of ventilation (and indoor exposures to poor air quality) on health and other relevant human responses. These measuring campaigns should include much better characterization of ventilation and exposure than was achieved earlier and should examine in detail the influence of indoor and outdoor sources of pollution on chronic health problems, and determine the environmental conditions responsible for the most severe exposures. Particular consideration should be given to people with special needs, such as patients with chronic respiratory diseases, the elderly, and children.
Let us conclude by quoting the 1964 version of “Basic principles of ventilation and heating” by Bedford. He wrote back then that “Great care is devoted to ensure that we have a pure water supply, and no one would suggest that in the interest of economy we should be doomed to drink polluted water. On aesthetic grounds alone, it should be one’s right to be allowed to live and work in a clean atmosphere which is free of objectionable odours”. Independently of Bedford, WHO [63] endorsed this opinion by publishing the document “The Right to Healthy Indoor Air”. This document states that “Under the principle of the human right to health, everyone has the right to breathe healthy indoor air.” Ventilation is and will continue to be one of the means to safeguard this principle. Therefore, we must agree on consistent principles and criteria for defining ventilation requirements in buildings occupied by people and follow them strictly. These criteria should consider different effects on building occupants and ensure that the systems are designed to fulfil their needs and are used efficiently. The paradigm change required should not only concern new design requirements but also new ventilation solutions and new ways to design, operate and maintain them that take account of all of the costs, not only the cost of energy but also the cost of the negative consequences of poor ventilation for health, productivity and socio-economic wellbeing. The new paradigm for ventilation in buildings should have every single building occupant at the centre of all recommendations.
This article is mainly based on a presentation made during the special workshop organized by REHVA at the CLIMA 2019 conference in Bucharest, Romania; parts of it were also included in a plenary talk at the Healthy Buildings Europe conference organized in 2017 by ISIAQ in Lublin, Poland. It includes the HealthVent project results supported by a grant from the European Commission, Executive Agency for Health and Consumers (Contract no 2009 12 18) and carried out between 2011 and 2013. Many thanks go to the entire HealthVent Team for their outstanding collaboration. Special thanks go to Prof. Olli Seppänen for his encouragement to prepare this article.
[1] Hänninen, Otto, et al. "Environmental burden of disease in Europe: assessing nine risk factors in six countries." Environmental health perspectives 122.5 (2014): 439-446.
[2] Zhang, X., et al. "The prevalence and incidence of sick building syndrome in Chinese pupils in relation to the school environment: a two‐year follow‐up study." Indoor air 21.6 (2011): 462-471.
[3] Seppanen, Olli A., and William J. Fisk. "Summary of human responses to ventilation." Indoor Air 14 (2004): 102–118.
[4] Sundell, Jan, et al. "Ventilation rates and health: multidisciplinary review of the scientific literature." Indoor air 21.3 (2011): 191-204.
[5] Wargocki, Pawel. "The effects of ventilation in homes on health." International Journal of Ventilation 12.2 (2013): 101-118.
[6] Carrer, Paolo, et al. "What does the scientific literature tell us about the ventilation–health relationship in public and residential buildings?." Building and Environment 94 (2015): 273-286.
[7] Yaglou CP, Riley EC and Coggins, DI. Ventilation requirements, ASHVE Transactions 42 (1936):133-162.
[8] Fanger, P. O., et al. "Air pollution sources in offices and assembly halls, quantified by the olf unit." Energy and Buildings 12.1 (1988): 7-19.
[9] Cain, William S., et al. "Ventilation requirements in buildings—I. Control of occupancy odor and tobacco smoke odor." Atmospheric Environment (1967) 17.6 (1983): 1183-1197.
[10] Iwashita, G. "Indoor air quality assessment based on human olfactory sensation." Journal of Architectural Planning and Environmental Engineering 410 (1990): 9-19.
[11] Berg-Munch, B., G. Clausen, and P. O. Fanger. "Ventilation requirements for the control of body odor in spaces occupied by women." Environment International 12.1-4 (1986): 195-199.
[12] Gunnarsen, Lars, and P. Ole Fanger. "Adaptation to indoor air pollution." Environment International 18.1 (1992): 43-54.
[13] ASHRAE, Standard. "62.1. 2007, Ventilation for Acceptable Indoor Air Quality." American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc., Atlanta, GA (2019).
[14] WHO. "Indoor Air Quality Research, Report on WHO Meeting, Euro‐Report and Studies 103." (1984).
[15] Mendell, Mark J. "Non‐specific symptoms in office workers: a review and summary of the epidemiologic literature." Indoor Air 3.4 (1993): 227-236.
[16] Sundell, Jan, Thomas Lindvall, and Berndt Stenberg. "Associations between type of ventilation and air flow rates in office buildings and the risk of SBS-symptoms among occupants." Environment International 20.2 (1994): 239-251.
[17] Fisk, William J. "Quantitative relationship of sick building syndrome symptoms with ventilation rates." Indoor Air 19, (2009): 159-165.
[18] Seppänen Olii A, et al. “Ventilation and performance in office work”. Indoor Air 16 (2006):28–36.
[19] Wargocki, Pawel, et al. "The relationships between classroom air quality and children’s performance in school." Building and Environment 173 (2020): 106749.
[20] Milton Don K, et al. “Risk of Sick Leave Associated with Outdoor Air Supply Rate, Humidification, and Occupant Complaints”. Indoor Air 10 (2000): 212–221.
[21] Shendell Derek G et al. “Associations between classroom CO₂ concentrations and student attendance in Washington and Idaho”. Indoor Air 14 (2004): 333–341.
[22] Mendell, Mark J., et al. "A longitudinal study of ventilation rates in California office buildings and self-reported occupant outcomes including respiratory illness absence." Building and Environment 92 (2015): 292-304.
[23] Morawska, Lidia, et al. "How can airborne transmission of COVID-19 indoors be minimised?." Environment international 142 (2020): 105832.
[24] Li Yuguo et al. “Role of ventilation in airborne transmission of infectious agents in the built environment – a multidisciplinary systematic review” Indoor Air 17 (2007):2–18.
[25] Rudnick, S. N., and D. K. Milton. "Risk of indoor airborne infection transmission estimated from carbon dioxide concentration." Indoor air 13.3 (2003): 237-245.
[26] Li, Yuguo, et al. "Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant." Building and Environment (2021): 107788. [27] Persily, Andrew. "What we think we know about ventilation." International Journal of Ventilation 5.3 (2006): 275-290.
[28] Persily, Andrew K. "Field measurement of ventilation rates." Indoor Air 26.1 (2016): 97-111.
[29] Seppänen, O. A., W. J. Fisk, and M. J. Mendell. "Association of ventilation rates and CO₂ concentrations with health and other responses in commercial and institutional buildings." Indoor air 9.4 (1999): 226-252.
[30] Satish, Usha, et al. "Is CO₂ an indoor pollutant? Direct effects of low-to-moderate CO₂ concentrations on human decision-making performance." Environmental health perspectives 120.12 (2012): 1671-1677.
[31] Allen, Joseph G., et al. "Associations of cognitive function scores with carbon dioxide, ventilation, and volatile organic compound exposures in office workers: a controlled exposure study of green and conventional office environments." Environmental health perspectives 124.6 (2016): 805-812.
[32] Allen, Joseph G., et al. "Airplane pilot flight performance on 21 manoeuvres in a flight simulator under varying carbon dioxide concentrations." Journal of exposure science & environmental epidemiology 29.4 (2019): 457-468.
[33] Kajtár, László, and Levente Herczeg. "Influence of carbon-dioxide concentration on human well-being and intensity of mental work." QJ Hung. Meteorol. Serv 116 (2012): 145-169.
[34] Zhang, Xiaojing, Pawel Wargocki, and Zhiwei Lian. "Human responses to carbon dioxide, a follow-up study at recommended exposure limits in non-industrial environments." Building and Environment 100 (2016): 162-171.
[35] Zhang, Xiaojing, et al. "Effects of exposure to carbon dioxide and bioeffluents on perceived air quality, self‐assessed acute health symptoms, and cognitive performance." Indoor air 27.1 (2017): 47-64.
[36] Fisk, William, Pawel Wargocki, and Xiaojing Zhang. "Do Indoor CO₂ Levels Directly Affect Perceived Air Quality, Health, or Work Performance?." ASHRAE Journal 61.9 (2019).
[37] Du, Bowen, et al. "Indoor CO₂ concentrations and cognitive function: A critical review." Indoor air 30.6 (2020): 1067-1082.
[38] EN, CEN Standard. "16798-1. Energy Performance of Buildings—Ventilation for Buildings—Part 1: Indoor Environmental Input Parameters for Design and Assessment of Energy Performance of Buildings Addressing Indoor Air Quality." Thermal Environment, Lighting and Acoustics—Module M1-6 (2019).
[39] Brelih, Nejc. "Ventilation rates and IAQ in national regulations." REHVA. Eur. HVAC. J 1 (2012): 24-28.
[40] Dimitroulopoulou, C. "Ventilation in European dwellings: A review." Building and Environment 47 (2012): 109-125.
[41] Asikainen, Arja, et al. "Reducing burden of disease from residential indoor air exposures in Europe (HEALTHVENT project)." Environmental Health 15.1 (2016): 61-72.
[42] Asikainen, Arja, et al. "The proportion of residences in European countries with ventilation rates below the regulation based limit value." International Journal of Ventilation 12.2 (2013): 129-134.
[43] Wargocki, Pawel, et al. "Ventilation and health in non-industrial indoor environments: report from a European multidisciplinary scientific consensus meeting (EUROVEN)." Indoor air 12.2 (2002): 113-128.
[44] Pettenkoffer, M. "Über den Luftwechsel in Wohngebäuden. Muenchen: Cottasche Buchhandlung." (1858).
[45] Carrer, Paolo, et al. "On the development of health-based ventilation guidelines: principles and framework." International journal of environmental research and public health 15.7 (2018): 1360.
[46] Sieber, W. Karl, et al. "The National Institute for Occupational Safety and Health indoor environmental evaluation experience. Part Three: Associations between environmental factors and self-reported health conditions." Applied Occupational and Environmental Hygiene 11.12 (1996): 1387-1392.
[47] Federspiel, C. C., et al. "Worker performance and ventilation in a call center: analyses of work performance data for registered nurses." Indoor air 14. (2004): 41-50.
[48] Viessman, Warren. "Ventilation control of odor." Annals of the New York Academy of Sciences 116.2 (1964): 630-637.
[49] Sundell, Jan. "Guidelines for Nordic building regulations regarding indoor air quality." Environment International 8.1-6 (1982): 17-20.
[50] Bornehag, Carl-Gustaf, et al. "Association between ventilation rates in 390 Swedish homes and allergic symptoms in children." Indoor air 15.4 (2005): 275-280.
[51] Engvall, K., P. Wickman, and D. Norbäck. "Sick building syndrome and perceived indoor environment in relation to energy saving by reduced ventilation flow during heating season: a 1 year intervention study in dwellings." Indoor air 15.2 (2005): 120-126.
[52] Erdmann, Christine A., and Michael G. Apte. "Mucous membrane and lower respiratory building related symptoms in relation to indoor carbon dioxide concentrations in the 100-building BASE dataset." (2004).
[53] World Health Organization (WHO). "Indoor Air Pollutants Exposure and Health Effects Report on a WHO Meeting Nördlingen, 8–11 June 1982." EURO reports and studies 78 (1982).
[54] WHO. “Air quality guidelines for Europe”. Copenhagen, WHO Regional Office for Europe, WHO Regional Publications, European Series, No. 23 (1987).
[55] World Health Organization. Air quality guidelines: global update 2005: particulate matter, ozone, nitrogen dioxide, and sulphur dioxide. World Health Organization, 2006.
[56] World Health Organization. "WHO guidelines for indoor air quality: selected pollutants." (2010).
[57] Sun, Yuexia, et al. "In China, students in crowded dormitories with a low ventilation rate have more common colds: evidence for airborne transmission." PloS one 6.11 (2011): e27140.
[58] Myatt, Theodore A., et al. "A study of indoor carbon dioxide levels and sick leave among office workers." Environmental Health 1.1 (2002): 1-10.
[59] Myatt, Theodore A., et al. "Detection of airborne rhinovirus and its relation to outdoor air supply in office environments." American journal of respiratory and critical care medicine 169.11 (2004): 1187-1190.
[60] Guo, Mingyue, et al. "Review and comparison of HVAC operation guidelines in different countries during the COVID-19 pandemic." Building and Environment (2020): 107368.
[61] ASHRAE, Standard. "Standard 170-2017-Ventilation of Health Care Facilities 1 (ANSI/ASHRAE/ASHE Approved), in." ASHRAE 170‐2017 (2017).
[62] Melikov, Arsen Krikor. "Advanced air distribution: improving health and comfort while reducing energy use." Indoor air 26.1 (2016): 112-124.
[63] World Health Organization. The right to healthy indoor air: report on a WHO meeting, Bilthoven, The Netherlands 15-17 May 2000. No. EUR/00 (5020494. Copenhagen: WHO Regional Office for Europe, (2000).
[64] Nielsen, Peter V., and Yuguo Li. "Ventilation." Encyclopedia of Environmental Health. Elsevier, 2019. 344-355.
[65] Mendell, Mark J., et al. "Environmental risk factors and work‐related lower respiratory symptoms in 80 office buildings: An exploratory analysis of NIOSH data." American Journal of Industrial Medicine 43.6 (2003): 630-641.
Follow us on social media accounts to stay up to date with REHVA actualities
0