Written by Olli Seppänen, President of FINVAC, former REHVA President
The original post was published on the FINVAC website on 15/01/2021
The need for good ventilation has been mainly justified with health reasons, but are there sound health criteria to rely on when defining appropriate ventilation rates? Göran Stålbom published a good summary about the history of ventilation criteria in the October 2020 newsletter of Swesiaq, the Swedish indoor air organization. The bottom line was that there are no scientific, widely accepted criteria for ventilation rates. The sizing practice has been largely based on various guideline values or on practical experience, meaning that at the end of the day proper ventilation performance may depend on the experience of the designer.
Perhaps, the most common rule of dimensioning ventilation systems in Europe and North America is based on the principle that ventilation has two basic components: the removal of contaminants from human sources and of emissions from building materials. The probably most widely used standards, EN 16798-1 and ASHRAE 62, use the sum of these two components as basis of ventilation design. These criteria depend on the odour of the room air and on the percentage of those who are statistically dissatisfied with the air quality. This principle was originally laid down by the Danish professor Ole Fanger. It was his idea to include emissions from building materials in air quality and ventilation criteria, which principle has resulted in significant emission reduction from building materials and ventilation equipment. However, with time these dimensioning criteria might have become outdated.
The above-mentioned standards were never accepted in all countries, partly due to their price for owners and users. The minimum ventilation value defined by authorities in Nordic countries is 6-7 L/s, per person. However, higher ventilation rates up to 10-20 L /s per person can be justified considering the impact ventilation has on occupants, such as productivity and SBS-symptoms (eg. the EU HealthVent project, see also final report). Indoor climate quality guidelines (e.g. the Finnish Indoor Climate Classification) recommend normally higher values for ventilation. In general, 10 L/s, per person is internationally considered as acceptable ventilation rate.
During this COVID-19 pandemic, we must yet again raise the question: is the ventilation in our buildings adequate to promote our health and protect us from diseases? Increasing evidence shows that airborne transmission is a major cause of virus spread, and this becomes even more important with the new virus variants on the rise which are much more infectious. A similar spread of airborne pathogens has been known in the past for other contagious diseases (e.g., influenza, measles, and tuberculosis).
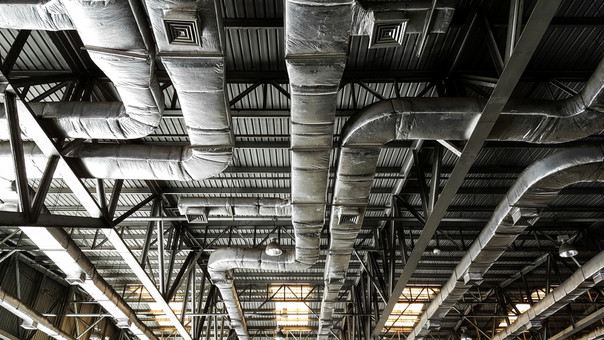
Increasing ventilation in existing buildings has been widely proposed to reduce coronavirus infections. The concentration of virus-carrying particles decreases approximately inversely with ventilation rate, but this does not make the air completely virus-free. Increasing ventilation also has its limits, both in old and new buildings. Old buildings use existing equipment with limited capacity. In new buildings, increasing ventilation is limited by investment and energy use. Therefore, we need other solutions to control infections caused by airborne pathogens.
The argumentation for the cleanliness of indoor air to breathe is lagging far behind the reasoning for clean domestic water for example. Water supply and sewage systems evolved rapidly after the mixing of sewage water with drinking water from wells was traced as the cause of cholera in England. Wastewater was carefully separated from drinking water, while health and hygiene requirements for domestic water developed rapidly. Should we learn from this example and apply it to ventilation technology? By analogy, mixing of exhaled air with inhaled air should be prevented. Clean, pathogen-free air should be supplied for breathing. Achieving this objective requires a new approach to ventilation efficiency, localized/personal ventilation, and air quality monitoring.
Localized indoor climate management has long been under development, especially in office environment, mainly related to work productivity, comfort, and energy efficiency. However, the technology is not widespread. Localized ventilation technology is familiar in hospital environment, especially in operating theatres and rooms for medical treatment. But there is a long way to go till we make sure that clean air technology is widely implemented in other building types and applications.
After all, ventilation should be optimally controlled to support the health of occupants. Ventilation should be increased if the potential emission of viruses rises in a space. A moderately good indicator of increased infection risk is CO2 concentration in the air. It is known that an infected person spreads more viral particles as the respiratory rate increases, while CO2-production also increases at the same time. CO2 -concentration is a proxy for particles transferred into the air by exhalation, especially with increasing physical activity, but it does not take into the account the use of voice. Virus release may increase a hundredfold as the volume of voice raises. Concerning the spread of infectious diseases and ventilation, it is an important factor whether people are sedentary or physically active, whether they speak loudly or are silent, such as in a cinema.
If CO2-concentration is used to control ventilation, we must take the characteristics of the room into greater account (delay in the concentration measurement, sensor location, air distribution etc.). It should also be noted that virus particles can be removed by air cleaning, in which case the CO2-concentration does not change while the virus concentration decreases.
Providing suitable ventilation based on the concentration and spread of pathogens results in different ventilation design than the current practice. Higher breathing rate increases the emission of and exposure to viral particles at the same time. Thus, elevated respiratory rate affects both the production of viral particles and the exposure, multiplying the risk of infection. In controlling the exposure, it may be more effective to remove exhaled air from the space as effectively as possible than increase ventilation.
It is time to change ventilation design from perceived air quality-based design to health-based ventilation design. Exhaled air must be effectively removed from inside and clean, pathogen-free air must be supplied for breathing. Ventilation and air distribution must be controlled according to occupants and their activities, not to the room space itself. A particular problem seems to be that some solutions which sound good in theory may not work in practice.
Read more on Indoor environmental quality and healthy buildings