Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
Preface from editor: Given the nature of this article and the intention to generate a feedback and dispute based on this article the RJ editor has with some help added some footnotes to stimulate reactions. The REHVA TRC installed recently a TF “IEQ requirements – input for revising EN 16798-1”, illustrating the interest of REHVA in addressing IEQ. |
|
Göran Stålbom |
Allmänna VVS Byrån AB /KTH Health informaticsgoran.stalbom@vvs-byran.se/gest@kth.se |
Paradigm shifts in science Thomas Kuhn, American philosopher of science, published The Structure of Scientific Revolutions in 1962. His statements are today more relevant than ever. Kuhn introduced the term paradigm shift and he made claims concerning the progress of scientific knowledge: 1. Scientific fields undergo periodic ”paradigm shifts” rather than solely progressing in a linear and continuous way. 2. The paradigm shifts opens new approaches to understand what scientists not considered valid before. 3. The notion of “a scientific truth”, at any given moment, cannot be founded solely by objective criteria, but is defined by a consensus of a scientific community. 4. Paradigms are often incommensurable, they present competing and contradictory versions of reality. 5. With a paradigm shift, new terminology is often created, which contributes to incommensurability. Kuhns conclusion was that our knowledge never can rely on ”objectivity” alone. Science must account for subjective perspectives. |
Contaminated indoor air can pose major health risks. This leads globally, according to the WHO, to a shortened life expectancy for more than three million people every year.[1] However, such serious risks are mainly associated with cooking indoors over open fireplaces. They are not primarily associated with inadequate ventilation. The problem in this case, is the design of the fireplaces and chimneys.
Public health should prioritize the obvious health risks, as well as the risks that can be easily remedied. The risks in kitchens associated with cooking and combustion are good examples. In Europe, the risks are significantly lower than the one mentioned above. But frying food without a good exhaust hood undoubtedly involves some risk.

Open fireplaces for cooking are a major smoke problem and a serious health risk in many countries.
Fireplaces, gas stoves, candles, especially scented candles, and other combustion activities can produce unpleasant and toxic air pollutants. Frequent and long indoor exposures from chain-smoking people is not risk-free. The use of cleaning products with unclear chemical content and other chemicals always requires caution. The warning texts should be heeded. Those who live close to industrial areas or next to a busy street should consider strategies for when window ventilation should take place, depending also on weather and wind.
For the residents, caution and good judgment is essential. It can be difficult to do more. One option for the anxious one may be to buy an effective air purifier.
The kind of risks that are mentioned should be paid more attention. At the same time, critical questions should be asked about many of the health and discomfort risks that have been highlighted since the 1980s. Are there discomfort risks that have been far too dramatized in an unfortunate interaction between politicians, media, researchers, authorities, and anxious people?
I wish my confidence in the research on “ventilation and health” in recent decades had been higher.
REHVA Journal observation #1: Countries like Sweden have done fantastic research over the last 50 years or so (just google Jan Sundell, Britta Berglund, Carl Gustav Bornehag, etc.). Also, other countries have been quite active in IA research (e.g. USA, Canada, Japan, China, Korea, Singapore, Australia, France, Germany, Denmark, Norway, Finland, ....) The research community is there (see e.g. www.isiaq.org). More research needed? Yes, but the problem is: 1. Lack of serious funding to conduct real large indoor air studies, 2. too little focus on transmission of infectious diseases via the air amongst IA researchers, 3. Authorities that don’t listen to what the indoor air community has to say.... |
But now there are reports from a new European research program, which started in 2010. The task was to elucidate the issues concerning “ventilation and health”. I hope their results will increase the knowledge. More on that later. First, an example of the new thinking of our time. In the REHVA Journal 2-2021, Pawel Wargocki writes:
“There are many beliefs regarding ventilation, and many are only partly true. Among the few, it is assumed that more ventilation will always improve indoor air quality, that low ventilation rate always means poor air quality, that it is simple to measure ventilation, that ventilation can be used as a metric predicting human responses, that outdoor air and air supplied indoors are clean, that ventilation systems are clean”
He further writes that buildings need ventilation that is
“reliable, flexible and well-functioning, adaptable, and responsive to different needs and unusual events”.
I agree with him. I believe also that we must abandon outdated ideas and find new relevant criteria for building ventilation. This requires, as he writes, “out-of-the-box thinking”.

Tobacco smoke has been a major comfort problem in indoor environments and above all a big health risk for the smoker. It is possibly the most disturbing and unhealthy indoor air pollution we have voluntarily been exposed to in modern times. It is now difficult to understand that smoking was generally accepted in indoor environments from the 1930s until around 2005. The picture shows the Swedish Prime Minister lighting his pipe at a press conference in 1973. Photo: Roger Tillberg/ TT.
The thinking since the 1980s that has long characterized the view of “ventilation and health” and have guided research, industry and authorities. It should have been abandoned long ago. I have stated this in many articles since the late 1990s.
Ventilation systems in modern buildings usually have a technology and design that shows they are primarily designed and built with a focus on creating comfort. The notion that our ventilation systems would be of great importance for health is well established. This is the case in industrial environments, but in offices and schools the function is primarily to avoid olfactory and thermal discomfort.
Now we seem to be facing a radical paradigm shift. Some health risks have been greatly exaggerated by the ventilation industry, authorities, and media with the support of outdated research. Fortunately, “ventilation and health” is now being brought to the attention of a new generation of researchers. An example is the Healthvent project that started in 2010. They approach the issue in a clear, wise, and balanced way. The focus seems good, and there are still important and principal questions to investigate and answer.
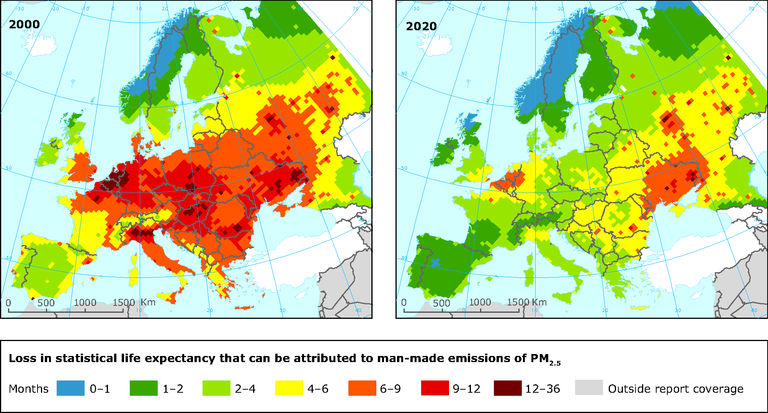
Particles PM2.5 are now known as a measurable air pollutant that poses a health risk to humans. The maps shows that the outdoor air content has clearly decreased. Source EEA 2016.
The new research changes the relationship between air quality and ventilation (air supply rate). So far, ventilation industry and authorities have had a strong focus on high air change rates.
REHVA Journal observation #2: At the same time many authorities focussed on Energy Performance which caused a reduction of air change. |
This doctrine has prescribed that with a certain minimum air change rate, all requirements for air quality will be met. But the Healthvent project seems to abandon this idea. Instead, the factual quality of the air (an exposure level) is presented as the central issue.
REHVA Journal observation #3: In this context it would make sense to focus more on performance requirements (e.g. in the form of maximum pollution levels that are allowed) than on means. |
They pay attention to measurable air pollutants listed in WHO guidelines. Details need to be discussed further. But it is a wise step forward, towards rationality.
The Healthvent project emphasizes the importance of source control and proposes a relatively low requirement for a “base ventilation rate”. This is 4 ℓ/s per person (equivalent to about 1 600 ppm CO₂).
REHVA Journal observation #4: Not sure if this understanding of base ventilation is correct, see how it was reported in EN 16798-1, tables B6-B14, “The HealthVent group also concluded that increasing outdoor air supply rates in non-industrial environments improves perceived air quality; that outdoor air supply rates below 25 l/s per person increase the risk of SBS symptoms, increase short-term sick leave, and decrease productivity among occupants of office buildings; and that ventilation rates above 0.5 air changes per hour (h−1) in homes reduce infestation of house dust mites in Nordic countries. |
The level was chosen to achieve a safety margin in accordance with current knowledge. This level: “will ensure no elevated risks for health due to exposure to human bioeffluents when all other pollutants meet the guideline values”.
But it is said that the level: “should be revised if more evidence on the effects of human bioeffluents become available, whether up or down”. Perhaps research will soon provide confirmation of what I see as proven experience – that bioeffluents are a comfort risk – not a health risk.[2]
Nowadays, we are well aware of the fact that viruses and other infectious agents are a significant indoor health risk. Different infectious agents have different strategies, which need to be studied further. The confusion surrounding ventilation and the Covid-19 shows that the Healthvent project also has a major task here. But it is important that such research is conducted without preconceived notions.[3]
In the preface to Wargocki's article in REHVA Journal 2-2021, five “incompletely resolved questions concerning ventilation” are listed. As I see it, they can-not yet be answered. What is required first is the agreement on what should be considered as objectives – and what to be means for achieving them. This must be clarified much better. The ventilation industry and authorities has too seldom made difference between objectives and means.
REHVA Journal observation #5: Correct performance based requirements (max values for PMx, CO2, TVOC…) should be the basis for our designs. |
Since the 1980s, modern technical systems have been considered necessary for health. Ventilation and air change rates have been perceived as objectives. Measured “statutory air change rate” has been considered the measure of good “air quality”.
This is unreasonable and must be reversed. The objectives should reasonably be air quality, health, well-being and comfort. Examples of means are source control, ventilation (air change), air purification and air cleaning. This is obvious to anyone who is active in the industry. Yet still too few, almost none, have reflected upon it. Even “purchased energy”, such as electricity, heating and cooling, are means, whose use must be limited with efficient systems, correct ventilation, temperature and operating times as well as utilization of the thermal dynamics of the building and the technical systems.
The benefits for “office work performance” and “school learning performance” is often presented as an objective for ventilation, but the causality is still unclear and requires more research.
The objectives, air quality, health,comfort and well-being, can be difficult to formulate and define. However, technical systems for ventilation are easy to plan, design, install, control and measure. We are easily seduced by the visible and the measurable. But the concepts of health, well-being and comfort are complex and elusive. There are established definitions - but they are debatable.[4] And the concept of “air quality” has been particularly difficult to define.
Large air change rates can sometimes provide thermal comfort. The ventilation industry and authorities have long argued that it is also important for health. Of course, this is the case in polluted environments, for example in industry. Not necessarily in schools and offices.
The term “air quality” has been used since 1967 for outdoor air. Later also for indoor environments, but still without an established definition. The term has been used in several different ways. The air quality criterion has been based on, for example:
· to achieve a minimum (outdoor) air change in a room (now common in Sweden),
· to measure selected air pollutants for which a maximum guideline value has been specified (WHO Guidelines referred by the Healthvent project),
· people's subjective perception of the quality of air (suggested by P.O. Fanger).
The concept of air quality has therefore to me remained vague and unclear and is often met with scepticism. In this text it is used in this traditional sense with the hope of better future terminology. Both meteorologists and indoor researchers nowadays often prefer to use its opposite, the more specific “air pollution”.
Air in ordinary buildings is in constant motion. It penetrates the windward wall, leaves from the leeward. Heating creates thermals. People move and breathe - the air swirls. Doors and windows are opened and closed. The sun affects. The Danish artist Vilhelm Hammershøi studied air movements with great interest. 1990 he painted “Dust Motes Dancing in Sunbeams”. Can “unventilated” spaces be created despite all this? If so, it has probably limited practical significance for health risks.
Harsh criticism can and should be directed towards older research and current guidelines, advice, and rules. I have presented these opinions previously in Swedish journals. This article is part of an ongoing discussion. I welcome critical comments to my interpretations and preliminary conclusions. Based on future objections, I will be happy to clarify and develop the reasoning further – and adjust if necessary. Our knowledge grows through constant critical review and necessary reconsideration.
REHVA Journal observation #6: Yes we guess that one of your points is that we should develop new models and new standards that are more performance based, that try to find a good balance between energy use (related to ventilation) and health/comfort on the other side, that address also the risk for transmission of infectious diseases via the air etc? |
Now it is time for the ventilation industry and authorities to begin the work to develop well-founded and useful guidelines based on proven experience and the science of our time.
[1] WHO, Burning Opportunity: Clean Household Energy for Health, Sustainable Development, and Wellbeing of Women and Children, 2016.
[2] Carrer et al, On the Development of Health-Based Ventilation Guidelines: Principles and Framework, 2018.
[3] Lidia Morawska et al.,A paradigm shift to combat indoor respiratory infection, Science 14 May 2021: Vol. 372, Iss. 6543, p. 689-691.
[4] Altomonte et al, Ten questions concerning well-being in the built environment, Building and Environment (2020),
Follow us on social media accounts to stay up to date with REHVA actualities
0