Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
Tomáš Fečer |
PhD, Department of Energy and Process Engineering, Norwegian University of Science and Technology, Trondheim, Norway |
|
|
|
Marina Asuero Von Munthe Af Morgenstierne | Yang Bi | Hans Martin Mathisen |
M.Sc, Department of Energy and Process Engineering, Norwegian University of Science and Technology | PhD student, Department of Energy and Process Engineering, Norwegian University of Science and Technology | PhD, Professor, Department of Energy and Process Engineering, Norwegian University of Science and Technology |
|
|
|
Trond Thorgeir Harsem | Liv-Inger Stenstad | Guangyu Cao |
MSc, Responsible Research & Development for HVAC, Norconsult | MSc, Radiographer and R&D coordinator, St. Olavs Hospital | Dr. (Sc.), Professor, Department of Energy and Process Engineering, Norwegian University of Science and Technology, Trondheim, Norwayguangyu.cao@ntnu.no |
Clean air in operation rooms (ORs) prevents surgical site infections (SSI) [1], which refer to infection at the skin, tissue, or organ level within 30 to 90 days of surgery [2]. Air currents and human movement in the surgical room can relocate the squames and bacteria-carrying particles (BCPs) towards the sterilised area [3], [4]. Studies have demonstrated that BCPs can be also spread around the surgical area due to thermal plumes and contaminate the surgical site [9]. Interaction between the skin of the human body and surrounding air creates a temperature gradient where the convective boundary layer (CBL) around the surfaces of the human body releases a thermal plume (TP) [5][6]. Therefore, thermal plumes (TP) are an energy exchange between the body and its surroundings, causing the air to rise slowly and transporting pollutants with less density than the supply air [7]. The thermal plume (TR) and the convective boundary layer (CBL) of the human body are studied through both numerical and experimental approaches without, and with a breathing manikin in small occupied spaces [5][6][9][9][10], isolation room [4], operating room with mixing, laminar airflow ventilation and their combination [7][11]. The interest to intervene in a significant way to understand the TP and CBL is obvious. Among those studies, there are three main aspects that influence the buoyancy effect of TP and CBL – the different temperatures between the skin and surrounding air, the body position of the manikin, and the velocity of air over the body.
Therefore, understanding the thermal plumes and interaction between different airflows is critical to recognising the airflow pattern in a room and thus the risk of SSI [12]. This study aims to quantify and characterise the impact of two different room temperatures, 21°C and 23°C, on the thermal plume around the patient wound in two different rooms of St. Olav’s hospital with mixing (MV) and laminar airflow (LAF).
Measurement of temperature, air velocity and turbulence intensity is executed in two operating rooms, MV and LAF with two different room temperatures, 21°C and 23°C, respectively. The operating room with mixing ventilation and 20 ACH has an area of 59.1 m² and a height of 2.9 m while the laminar operating room with 61 ACH has a total area of 56.1 m², of which 11 m² is the rectangular LAF zone, with a room height of 3.08 m.
A female humanoid thermal manikin is 1.7 m tall and located at an operating bed to simulate a patient under stomach surgery. The manikin is covered by the surgical blanket and at the surgical site is cut into the shape of a 20 cm square. The surface temperature of the patient’s wound is in the range of 33.5 to 34.5°C measured by the image of the thermal detector Bosch PTD 1 and infrared camera Flir one - iOS.

Figure 1. In the left, image of the mixing ventilation operating room at St. Olav. In the right, Image of the Laminar airflow operating room at St. Olav Hospital.
The sides of the surgical blanket is taped to the manikin as seen in Figure 2. The interrogation area of 100cm (height) x 60cm (width) around the wound is measured by seven anemometers SensoAnemo 5100 LSF, 8.5 cm apart, in levels 5, 10, 25, 50, and 100 cm over the wound. Each level is measured for five minutes. Boundary conditions of measurement cases are introduced in the Table 1.

Figure 2. In the left, illustration of anemometers measurement and size of surgical wound. In the right, scheme of measuring points.
Table 1. Measuring cases.
Case No. | Type of ventilation [-] | Room temperature [°C] | Supply temperature [°C] | ACH |
Case (a) | MV | 21 | 18.9 | 20 |
Case (b) | MV | 23 | 23.3 | 20 |
Case (c) | LAF | 21 | 21.2 | 61 |
Case (d) | LAF | 23 | 22.8 | 61 |
Figure 3 represents the velocity results of four scenarios, where cases, (a) and (b), refer to MV and cases (c) and (d) represent LAF. The thermal plume for the case (a), has the highest velocity at 10 cm above the wound. The thermal plume’s velocity decreases with increasing distance from the wound and mixes with the room air, which is caused by the gradual weakening of the buoyancy effect, respectively. For the case (b) the velocity is lower in the vertical direction than the horizontal direction, which is also proven by temperature stratification in Figure 5. In case (c) a higher velocity gradient occurs within 50 cm over the patient’s wound than in case (d), which is caused by higher interaction of thermal plume by LAF. In the case (d), due to the lower temperature difference and density difference between laminar airflow and thermal plume, their interaction is observed closer to the wound.

Figure 3. Velocity profile of the patient´s thermal plume of mixing ventilation (a), (b) and laminar airflow (c) and (d).
Turbulent intensity and temperature are also observed for all four scenarios, case (a), (b), (c) and (d) which are shown in Figure 4 and Figure 5, respectively. Due to higher room temperature in this case (b) by 2°C, Figure 4 shows that a weaker buoyancy effect occurs, and the thermal plume expands in a horizontal direction. In both LAF cases (c) and (d), laminar airflow is dominated against the buoyancy effect of the thermal plume, respectively. In Figure 4, the maximum values of turbulence intensity are observed in the LAF of 40% of cases (c) (d), which are very close to the patient’s wound. However, cases of MV (a) and (b) indicate an overall higher gradient of turbulence intensity in the horizontal and vertical directions. In case (a) on both sides is occurs locations with TI up to 23% cause a rising thermal plume, which is possibly observed in the centre of the temperature field. In case (b) is observed area in the vertical direction on the left side and in the upper part of TI up to 30%. This is caused by the expansion of the thermal plume in the horizontal direction and low velocities over the thermal plume which is also observed by stratification on the temperature field. As is mentioned in the previous chapter, case (c) has higher TI above and around the surgical wound than case (d) due to the higher interaction of the thermal plume with LAF.

Figure 4. Turbulence intensity profile of the patient´s thermal plume of mixing ventilation (a), (b) and laminar airflow (c) and (d).
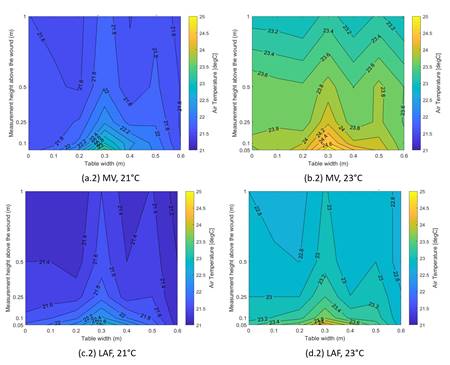
Figure 5. Temperature profile of the patient´s thermal plume of mixing ventilation (a), (b) and laminar airflow (c) and (d).
This study shows an experimental investigation of the interaction of thermal plumes with mixing and laminar airflow over a patient´s wound at two room temperatures, 21°C and 23°C. By comparing the results of air velocity, temperature, and turbulence intensity of four cases for MV (a), (b) and for LAF (c), (d), the conclusions are summarised as follows:
a) In the cases with a room temperature of 23°C, (b) and (d) observed the expansion of the thermal plume in the horizontal direction, while with a room temperature of 21°C thermal plume directly expanded in the vertical direction.
b) In the case of laminar airflow, a higher room temperature, 23°C, indicates lower turbulence intensity over the patient's wound and surroundings.
c) In the case of mixing ventilation, a lower temperature, 21°C, indicates lower turbulence intensity over the patient's wound and surroundings.
d) Laminar airflow has higher turbulence intensity within 25 cm over the wound than mixing ventilation, while the turbulence intensity with mixing ventilation varies in both vertical and horizontal directions.
[1] O. M. Lidwell, E. J. Lowbury, W. Whyte, R. Blowers, S. J. Stanley, and D. Lowe, “Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: A randomised study.,” BMJ, vol. 285, no. 6334, pp. 10–14, 1982, issn: 0007-1447. doi: 10.1136/bmj.285.6334.10. eprint: https://www.bmj.com/content/285/6334/10.full.pdf. [Online]. Available: https://www.bmj.com/content/285/6334/10.
[2] J. Liston and A. Bayles, “Surgical site infections,” Surgery (Oxford),vol. 41, no. 2, pp. 65–70, 2023, issn: 0263-9319. doi: https://doi.org/10.1016/j.mpsur.2022.11.009. [Online]. Available: https://www.sciencedirect.com/science/article/pii/S0263931922002411.
[3] Sun, S., Li, J. & Han, J. How human thermal plume influences near-human transport of respiratory droplets and airborne particles: a review. Environ Chem Lett 19, 1971–1982 (2021). https://doi.org/10.1007/s10311-020-01178-4.
[4] Yang, C., Yang, X. & Zhao, B. The ventilation needed to control thermal plume and particle dispersion from manikins in a unidirectional ventilated protective isolation room. Build. Simul. 8, 551–565 (2015). https://doi.org/10.1007/s12273-014-0227-6.
[5] Shuzo Murakami, Shinsuke Kato, Jie Zeng, Combined simulation of airflow, radiation and moisture transport for heat release from a human body,Building and Environment,Volume 35, Issue 6, 2000, Pages 489-500, ISSN 0360-1323, https://doi.org/10.1016/S0360-1323(99)00033-5.
[6] Licina D, Melikov A, Sekhar C, Tham KW. Human convective boundary layer and its interaction with room ventilation flow. Indoor Air. 2015 Feb;25(1):21-35. doi: 10.1111/ina.12120. Epub 2014 May 24. PMID: 24750235.
[7] Laurențiu Tacutu, Florin Bode, Ilinca Năstase, Cristiana Croitoru & Angel Dogeanu (2022) Experimental and numerical study on the thermal plumes of a standing and lying human in an operating room, Science and Technology for the Built Environment, 28:1, 2-20, https://doi.org/10.1080/23744731.2021.1963133.
[8] Guohui Feng, Yang Bi, Yixian Zhang, Yilin Cai, Kailiang Huang, Study on the motion law of aerosols produced by human respiration under the action of thermal plume of different intensities, Sustainable Cities and Society, Volume 54, 2020, 101935, ISSN 2210-6707, https://doi.org/10.1016/j.scs.2019.101935.
[9] Jianchao Ma, Hua Qian, Peter V. Nielsen, Li Liu, Yuguo Li, Xiaohong Zheng, What dominates personal exposure? Ambient airflow pattern or local human thermal plume, Building and Environment, Volume 196, 2021, 107790, ISSN 0360-1323, https://doi.org/10.1016/j.buildenv.2021.107790.
[10] Zhu Cheng, Cao Guangyu, Amar Aganovic, Li Baizhan, Experimental study of the interaction between thermal plumes and human breathing in an undisturbed indoor environment, Energy and Buildings, Volume 207, 2020, 109587, ISSN 0378-7788, https://doi.org/10.1016/j.enbuild.2019.109587.
[11] Zhijian Liu, Di Yin, Yunfei Niu, Guoqing Cao, Haiyang Liu, Liangqi Wang, Effect of human thermal plume and ventilation interaction on bacteria-carrying particles diffusion in operating room microenvironment, Energy and Buildings, Volume 254, 2022, 111573, ISSN 0378-7788, https://doi.org/10.1016/j.enbuild.2021.111573.
[12] P. Danc˘a, A. Jamin, I. Nastase, B. Janssens, W. Bosschaerts, and C.Co¸soiu, “Experimental and numerical study of the flow dynamics and thermal behavior inside a car cabin: Innovative air diffusers and human body plumes interactions,” Energy Reports, vol. 8, pp. 992–1002, 2022, Technologies and Materials for Renewable Energy, Environment and Sustainability, issn: 2352-4847. doi: https : / / doi . org / 10 . 1016 / j . egyr . 2022 . 07 . 133. [Online]. Available: https://www.sciencedirect.com/science/article/pii/S2352484722014007.
Follow us on social media accounts to stay up to date with REHVA actualities
0