Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
|
|
Jarek Kurnitski | Pawel Wargocki | Amar Aganovic |
REHVA Technology and Research Committee, Tallinn University of Technology, Tallinn, Estoniajarek.kurnitski@ttu.ee | Department of Civil Engineering, Technical University of Denmark, Copenhagen, Denmark | Department of Automation and Process Engineering, UiT The Arctic University of Norway, Tromsø, Norway |
In the context of COVID-19, the effect of indoor relative humidity (RH) on infection risk has been extensively discussed. This has brought RH effects under the attention of researchers and practitioners and has resulted in new experimental evidence and awareness-raising. Before COVID-19, scientific discussion on RH effects has had decreasing trend, many positive and negative effects are listed, but no clear decisions concerning IEQ control have been drawn. RH has been addressed in EN 16798-1 and ISO 17772-1 standards with a recommendation that humidification and dehumidification in European climates are generally unnecessary. However, the discussions on RH concerning the COVID-19 deserve reiteration of what we know about RH and its effects on humans.
Generally, RH and temperature contribute to the infection risk by three main mechanisms:
· By affecting the virus viability, i.e., the length of inactivation time of the virus in the air;
· By impacting expelled droplets and aerosol desiccation and residence time in the air;
· By influencing the susceptibility of people through the sensitivity of nasal systems and mucous membranes.
Several studies have indicated that RH and temperature significantly influence the incidence of COVID-19 for a specific location (Mecenas et al. 2020, Tobías et al. 2021, Yuan et al. 2021), sharing common findings that colder and drier climates may increase the incidence of COVID-19. Although several recent experimental studies have been relating the survival of the SARS-CoV-2 virus in aerosols under various RH and temperature conditions (Dabisch et al. 2020, Schuit et al. 2020, Smither et al. 2020), the precise nature of the relationships is much less clear. On the contrary, the relationship between deposition loss by gravitational settling and RH is clear: the deposition loss of infectious particles is determined by the droplets settling or terminal velocity, which itself is dependent on the size of the droplet. When released from the respiratory tract (assumed to have ~99.5% RH), droplets experience rapid evaporation and shrinkage upon encountering the unsaturated ambient atmosphere. The ultimate size of a droplet depends on ambient humidity, and size determines aerodynamic behaviour and whether the droplet will settle to the ground quickly or remain suspended in the air long enough to possibly cause a secondary infection. It has been suspected that due to low RH, the droplets that will evaporate to a smaller size could lead to more airborne suspension time of viral droplets, and ultimately, they could be transported to farther distances depending on ventilation conditions. However, the droplet desiccation is a fast process, for instance, an original droplet size of 10 µm will evaporate in 0.1 seconds and RH effect on shrinking is quite limited, as shown in Figure 1.
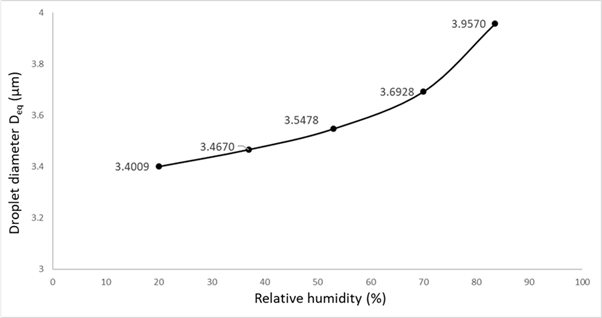
Figure 1. Equivalent dehydrated droplet diameter at five RH values (RH = 20%, 37%, 53%, 70% and 83.5%) for an original droplet size of 10 µm the indoor air temperature range 20-25°C (Aganovic et al. 2021).
The dependence of the equilibrium size of an aqueous droplet containing dry solutes on RH is described by one of the fundamental interpretations of equilibrium thermodynamics, also known as the Köhler theory (1936). Therefore, without incorporating the impact of RH, current modifications of the Wells-Riley model used to estimate infection risk are limited to only one specific RH assessment of the removal terms by inactivation and gravitational settling.
The wide ranges of RH values as defined by existing building regulations design criteria for humidity in both the U.S. (RH < 65% as per ASHRAE 2013) and Europe (20 < RH < 70% used for existing buildings as per EN 16798-1) together with the intensified sensitivity of nasal systems and mucous membranes to infections at low RH of 10-20% (Salah et al. 1988, Kudo et al. 2019) emphasizes the need for incorporating the variability of RH values in epidemiological models for a more accurate prediction of airborne transmission risks of SARS-CoV-2 in confined spaces. Consequently, by addressing these factors, a novel model for calculating the infection risk of airborne infectious transmission of SARS-CoV-2 as a function of RH was introduced in a recent paper (Aganovic et al., 2021). To advance a mechanistic understanding of the role of RH in aerosol transmission, the change in the size of respiratory droplets and aerosols and SARS-CoV-2 airborne decay at RHs ranging from 20% to 83.5% was modelled. Based on these results, the dynamics of droplets emitted from an infected person in an indoor environment were further modelled to simulate the airborne transmission of SARS-CoV-2 viral load, considering removal by ventilation, deposition by gravitational settling, and biological decay of the SARS-CoV-2 virus in aerosols. Such modelling can support public health experts, engineers, and epidemiologists in a more comprehensive understanding of the impact of RH on the infection risk in indoor spaces.
To characterize the impact of relative humidity on inactivation rate, experimental data on the survival time of SARS-CoV-2 in aerosols can be aggregated from measured values of k (min-1) currently available at RH 20% to 83.5%, Figure 2.
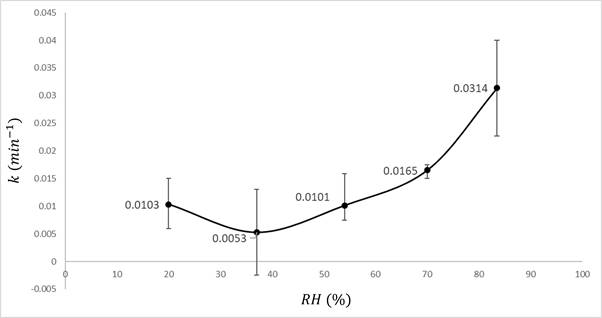
Figure 2. Mean, min, and max IAV inactivation rates (k) for each RH were derived based on experimental data adapted from Dabisch et al. (2020), Schuit et al. (2020), and Smither et al. (2020).
A modified version of the Wells-Riley model was used in (Aganovic et al. 2021) to include the impact of RH on the volume emission of respiratory droplets from an infected individual and its removal mechanisms of deposition by gravitational settling and inactivation by biological decay. This study was thus able to determine and estimate the magnitude by which RH can affect the airborne transmission of SARS-CoV-2 and reduce the infection risk from one infected individual within public indoor spaces. In addition to the impact of RH, by using updated characteristics of the SARS-CoV-2 virus on estimated infection dose, theoretical calculations of the infection risk were possible to perform for different scenarios considering the viral load in the infected individual, different size ranges of dehydrated respiratory droplets, and different ventilation rates, Figure 3.
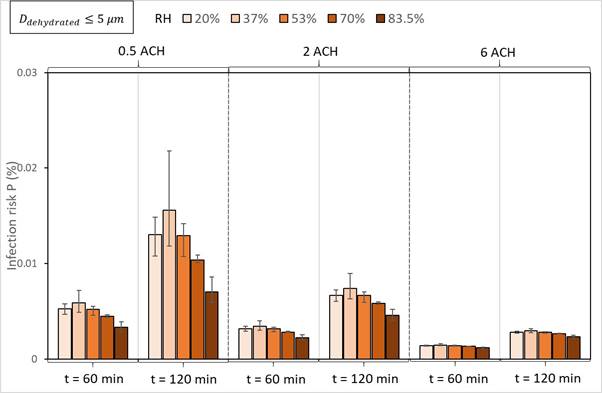
Figure 3. Impact of RH and ventilation on the infection risk probability P (%) when an infected person with a viral load of cv = 109 RNA/ml is speaking continuously for 60 and 120 min. The columns depict mean P (%), and the error bars present min and max values (Aganovic et al., 2021).
The infection risk P (%) will decrease with decreasing RH to 20% or by increasing from 37% to 83.5%, but mainly for RH > 53%, given the same ventilation rate, droplet size range, and viral load considered. For smaller droplets considered (Ddehyd ≤ 5 µm), the mean infection risk for 20% and 53% are approximately equal. The difference in infection risk for different RH values will increase with exposure time at a constant ventilation rate. The differences between infection risks for different RH values become relatively small for higher ventilation rates, and RH will have only a minor effect if any. Generally, increasing ventilation rate will provide a stronger effect in reducing infection compared to changing the relative humidity given the same exposure time and viral load considered. Changing RH in the range between 20% and 53% is ineffective plausibly due to the non-linearity of the relationship between RH and inactivation rates.
To explain the results in Figure 3, the removal efficiencies for all three mechanisms for different size ranges and ventilation rates are reported in Figure 4. Regardless of ventilation rate and droplet size considered, both the removal efficiency due to settling and inactivation increase at RH from 37% to 83.5%. The mean removal efficiency at RH = 20% will be higher than at RH = 53% for smaller droplets (Ddehyd ≤ 5 µm). At this size range, the differences in inactivation rates for different RH values will determine the overall impact of RH on the removal efficiency, as the removal efficiency for ventilation is not influenced by RH. At the same time, the differences in removal efficiency for settling for different RH are too small to impact the overall removal efficiency. However, as larger droplets have greater settling velocities at higher RHs, the equilibrium droplet size will be relatively larger and will therefore accelerate the removal mechanism. Thus, with an increase in the considered droplet size range, the relative removal efficiency effect by settling will increase. Although the difference between the settling removal efficiencies at different RH will increase with an increase in droplet size range, these differences will have a small impact compared with the overall removal efficiency at higher ventilation rates, as the ventilation rate removal efficiency is independent of RH value.
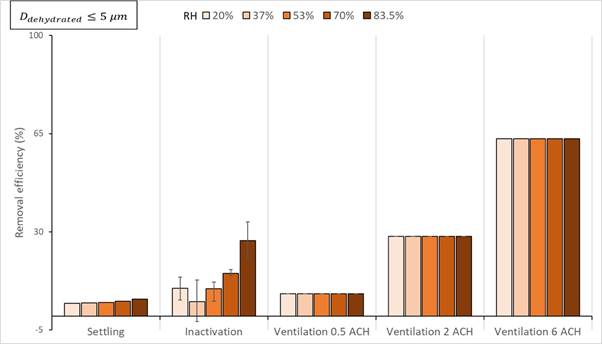
Figure 4. Removal efficiency when individual stopped speaking (source absent) due to gravitational settling, inactivation, and three different ventilation rates (0.5, 2, and 6 ACH) for small airborne infectious droplets (≤ 5 µm). The columns depict mean removal efficiency, and the error bars present min and max values (Aganovic et al., 2021).
The evaluation of the infection risk in Figures 3 and 4 does not consider the human immune system’s reaction to changes in RH. In this area, the evidence on RH effects is somewhat conflicting and not complete as studies provide an indication that the lower limit of RH could be 10%, 20%, or 30% RH. The sensitivity of nasal systems and mucous membranes has been extensively studied. Andersen et al. (1974) did not observe changes in mucociliary clearance during 78 hours of exposure to dry unpolluted air at 9% compared to 50% RH. Other studies showed that nasal systems and mucous membranes are more sensitive to infections at RH of 10-20% (Salah et al. 1988, Kudo et al. 2019). It is well established that low RH aggravates the eye tear film leading to eye symptoms like dry eyes, for which Wyon et al. (2006) showed significant differences between 25% and 15% RH. The dry nose and throat sensation also occurs in the nose and throat after some latency and without pollution, which is more pronounced at RHs below 10% (Wolkoff 2018). Therefore, some humidification in winter may sometimes be useful to reach the levels of 20-30% recommended in ISO 17772-1:2017 to be used as a design criterion if humidification systems are installed.
On the other hand, the use of humidifiers is linked with increased short-term sick-leave rates due to infections (Milton et al. 2001). Humidification is an energy-intensive process that may lead to wet surfaces in air conditioning systems, known as one of the most significant IAQ risk factors. Adding humidification to reduce sensitivity to infections may not be as beneficial as claimed, although it must be admitted that sensitivity to dry air in polluted air is increased (Andersen et al., 1974). Consequently, improved ventilation may provide the benefits of removing and diluting the viruses and reducing sensitivity, especially when RH levels are low.
It should also be noted that high RH (over 40-50% RH) may be harmful, especially during the winter. High humidity levels can lead to risk of mold and allergic reactions related to house dust mite. Indoor air humidity may condense on cold surfaces and increase the risk of microbial growth on surfaces, and further in structures, and deteriorate indoor air quality. Condensation of moisture, particularly on window panes, has been related to the indoor air problems linked to inadequate ventilation or wrong pressure difference over the building envelope in many studies. Moisture damages due to high indoor air humidity are, however, not so common as damages caused by other sources of water.
Evidence on the RH effect can be summarized in the following key points:
· The relative importance of RH and the ventilation rate in reducing the infection risk of the COVID-19 is comprehensively studied, allowing informed decisions to be made for indoor environmental control;
· The evidence clearly shows that humidification to moderate levels of 40% to 60% RH should NOT be expected to provide significant effects in reducing infection risk;
· High humidity levels can lead to risk of mold and allergic reactions related to house dust mite;
· Hence, installing and running humidifiers may NOT be an efficient solution to combat the infection risk in indoor spaces;
· The results emphasize the key role of ventilation in controlling the virus concentration in the air;
· Nasal systems and mucous membranes are more sensitive to infections at RH below 20% leading to dry eyes, nose, and throat sensation that supports to avoid excessively low RH, especially in cold winters;
· Technical means to address very small humidification need to 20% RH limit do not need to be humidifiers, but humidity recovery by proper selection of enthalpy or other hygroscopic heat exchangers may also be considered.
EN 16798-1:2019 Energy performance of buildings - Part 1: Indoor environmental input parameters for design and assessment of energy performance of buildings addressing indoor air quality, thermal environment, lighting, and acoustics CEN (2019).
ISO 17772-1:2017 Energy performance of buildings — Indoor environmental quality — Part 1: Indoor environmental input parameters for the design and assessment of energy performance of buildings.
Mecenas P., Bastos R., Vallinoto A.C.R., Normando D. Effects of temperature and humidity on the spread of COVID-19: A systematic review. PLoS One. 2020;15(9) (e0238339. PubMed PMID: 32946453. PMCID: PMC7500589. Epub 2020/09/19).
Tobías A, Molina T, Rodrigo M, Saez M. Meteorological factors and incidence of COVID-19 during the first wave of the pandemic in Catalonia (Spain): A multi-county study. One Health. 2021 Jun;12:100239. DOI: https://doi.org/10.1016/j.onehlt.2021.100239. Epub 2021 Mar 29. PMID: 33816746; PMCID: PMC8007195.
Yuan J, Wu Y, Jing W, et al. Association between meteorological factors and daily new cases of COVID-19 in 188 countries: A time series analysis. Sci Total Environ. 2021;780:146538. doi: https://doi.org/10.1016/j.scitotenv.2021.146538.
Dabisch P, Schuit M, Herzog A, Beck K, Wood S, Krause M, Miller D, Weaver W, Freeburger D, Hooper I. 2020. The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols. Aerosol Science and Technology 55(2):1–15.
Schuit M, Ratnesar-Shumate S, Yolitz J, Williams G, Weaver W, Green B, Miller D, Krause M, Beck K, Wood S. 2020. Airborne SARS-CoV-2 is rapidly inactivated by simulated sunlight. Journal of Infectious Diseases 222(4):564–571 DOI https://doi.org/10.1093/infdis/jiaa334.
Smither SJ, Eastaugh LS, Findlay JS, Lever MS. 2020. Experimental aerosol survival of SARS-CoV- 2 in artificial saliva and tissue culture media at medium and high humidity. Emerging Microbes & Infections 9(1):1–9.
Aganovic A, Bi Y, Cao G, Drangsholt F, Kurnitski J, Wargocki P. Estimating the impact of indoor relative humidity on SARS-CoV-2 airborne transmission risk using a new modification of the Wells-Riley model. Building and Environment 205 (2021) 108278. https://doi.org/10.1016/j.buildenv.2021.108278.
Köhler, H., “The nucleus in and the growth of hygroscopic droplets,” Trans. Faraday Soc. 32, 1152–1161 (1936).
ANSI/ASHRAE, 2013b. ANSI/ASHRAE Standard 169-2013, Climatic Data for Building Design Standards 8400, 104.
Salah et al., 1988. Nasal mucociliary transport in healthy subjects is slower when breathing dry air. European Respiratory Journal 1(9): 852-855.
Kudo et al., 2019. Low ambient humidity impairs barrier function and innate resistance against influenza infection. PNAS: 1-6.
Andersen, I. B., Lundqvist, G. R., Jensen, P. L., & Proctor, D. F. (1974). Human response to 78-hour exposure to dry air. Archives of Environmental Health: An International Journal, 29(6), 319-324.
Wolkoff P, 2018. Indoor air humidity, air quality, and health – An overview. International Journal of Hygiene and Environmental Health 221 (2018) 376–390.
Wyon, D.P., Fang, L., Lagercrantz, L., Fanger, P.O., 2006. Experimental determination of the limiting criteria for human exposure to low winter humidity indoors (RP-1160). HVAC&R Res. 12, 201–213.
Milton et al., 2001. Risk of Sick Leave Associated with Outdoor Air Supply Rate, Humidification, and Occupant Complaints. Indoor Air 2001. https://doi.org/10.1034/j.1600-0668.2000.010004212.x.
Follow us on social media accounts to stay up to date with REHVA actualities
0